For more information about cancer screening in BC, visit http://www.bccancer.bc.ca/screening.
This document includes information about:
- Breast Screening
- Cervix Screening
- Colon Screening
- Lung Screening
Full text:
BC Cancer Screening
Guidelines
Version: September 2023
BC Cancer Screening Guidelines 2
In British Columbia, there are four
province-wide screening programs:
For more information about cancer screening, visit http://www.bccancer.bc.ca/screening.
Breast Screening
Cervix Screening
Colon Screening
Lung Screening
BC Cancer Screening Guidelines 3
Support Your Patient’s Participation in
Screening
Health professionals play an important role in supporting their patients’ participation in cancer screening.
When you discuss the purpose of screening, benefits and risks, what to expect, and recommendations
with your patients, you can strongly impact their decision and improve the quality of their care and overall
experience. The way you explain the results and additional tests can also influence their adherence to followup
care and routine screening.
One way to start the conversation about screening is by asking your patient: “I’d like to talk to you today about
[type] screening. Before we begin, could you tell me what you already know or have heard about [type]
screening?” Their response will allow you to determine their initial understanding about screening and build
the conversation around new or clarifying information, which will support their decision to screen. Listen for
any fears, concerns, or traumas the patient may have or have heard others experience that could shape how
you engage them in the discussion.
Look for the Conversation Tip icon throughout the Guidelines for discussion prompts and
reminders.
What is the purpose of cancer screening?
Cancer screening means finding cancer or signs of cancer early, before symptoms appear, when it is likely
more treatable.
What are the benefits of cancer screening?
• Can help prevent certain types of cancer: Detecting, treating or removing precancerous lesions in the
cervix and colon can prevent them from developing into cancer.
• Can help detect cancer at its earliest stages: Finding cancer early means that it is less likely to have spread
and treatment can start earlier in the course of the disease. This allows for more treatment options and a
better chance of recovery.
What are the risks of cancer screening?
• False positives: Results may indicate an abnormality when there is none. This may lead to unnecessary
follow-ups, sometimes surgery, and cause increased stress and anxiety during this time.
• False negatives: Results may be normal when there are precancerous or cancerous lesions present. This
may lead to missed or delayed diagnoses and/or treatments.
• Over diagnosis: Results may find cases of cancer that are very slow growing and are not expected to
cause any problems during the patient’s lifetime. This may lead to treatment that may not benefit or have
unintended consequences for the patient.
• False reassurance: A negative result does not mean that the patient is at lower risk of cancer.
If your patient has a negative result, encourage them to monitor their health, be aware of any
unusual changes, and continue behaviours that will lower their cancer risk, including returning
for routine screening when they are due. Remind them to schedule an appointment with you if
they experience any symptoms.
BC Cancer Screening Guidelines 4
• Pain or discomfort: The patient may experience uncomfortable pressure during a mammogram, or
discomfort and/or bleeding during and/or after a Pap test.
• Exposure to radiation: The benefits of regular breast and/or lung screening outweigh the risks posed by
the small amount of radiation the patient is exposed to. The chances of getting cancer through repeated
radiation exposure is very low.1
• Unintended complications from diagnostic or follow-up test:
— Breast screening: Possible risks from a breast biopsy include an allergic reaction to the
anesthetic/freezing (highly unlikely if the patient has received freezing with no reaction
previously, such as at the dentist), infection at the biopsy site, bleeding from the biopsy site, not
getting a sample of the abnormal tissue, dizziness, and fainting. Biopsies may leave a scar that
fades over time. The patient may be called back for additional imaging or procedures.
— Cervix screening: Follow-up for cervical abnormalities, including colposcopy, may cause
pinching or cramping sensations during the procedure, or lead to long-term consequences for
future pregnancy (pre-term birth or low birth weight).
— Colon screening: Complications from a colonoscopy may include a reaction to the bowel
preparation or medication used for sedation, heart or lung problems, an infection, bleeding
from the colon and/or perforation of the colon (hole in the colon).
— Lung screening: The patient may feel some soreness or discomfort after a lung biopsy and may
need to rest for 1 to 2 days. Rare but possible risks of a lung biopsy include bleeding, infection
or a pneumothorax (collapsed lung).
What can your patient do to lower their cancer risk?
• Practice sun safety
• Quit commercial tobacco
• Be physically active
• Eat a balanced diet
• Maintain a healthy weight
• Reduce exposure to air pollution and radon
• Limit alcohol consumption
• Get vaccinated
• Go for routine cancer screening
For more information about cancer prevention, visit http://www.bccancer.bc.ca/prevent/.
1 Rampinelli C, De Marco P, Origgi D, et al. Exposure to low dose computed tomography for lung cancer screening and risk of cancer: secondary analysis of
trial data and risk-benefit analysis. BMJ. 2017;356:j347.
BC Cancer Screening Guidelines 5
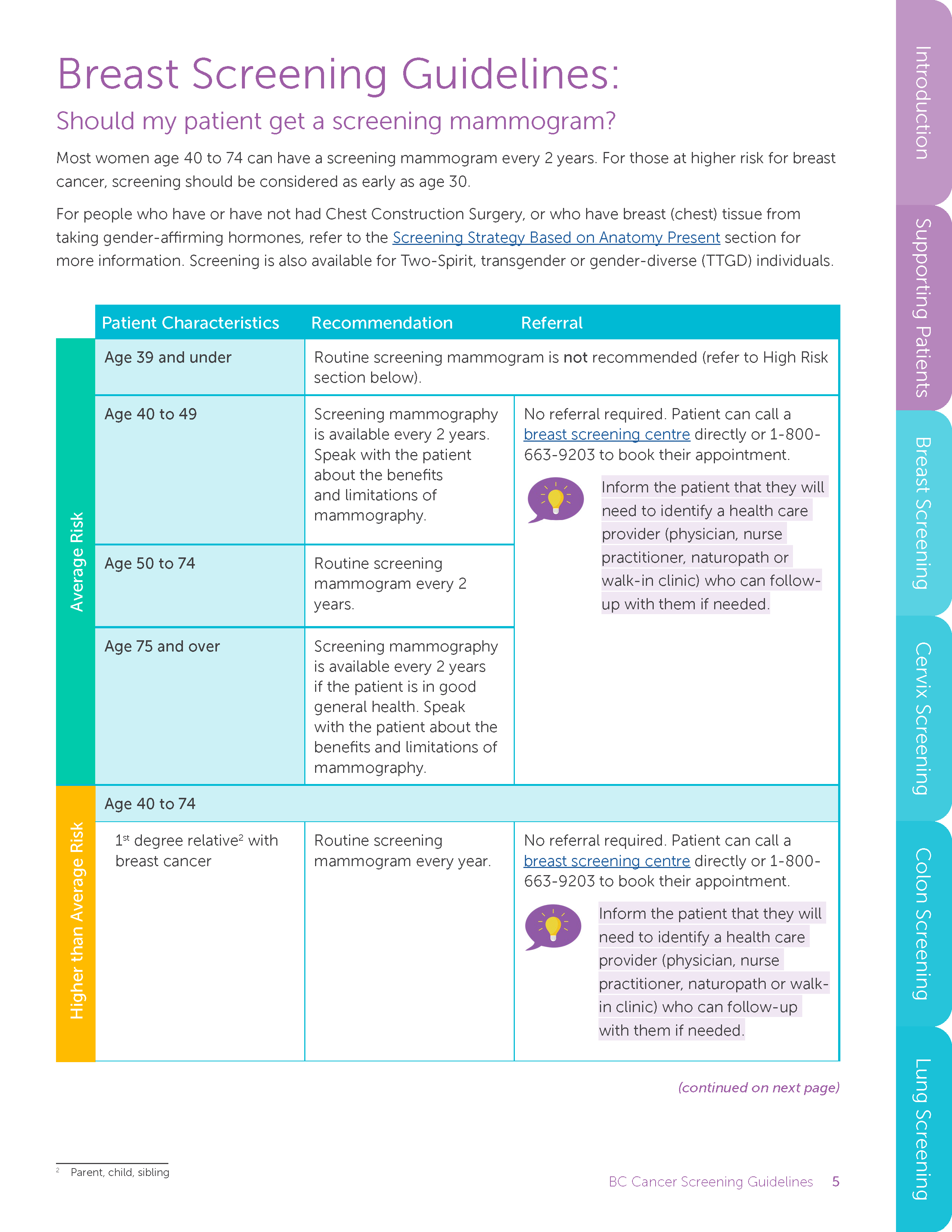
Breast Screening Guidelines:
Should my patient get a screening mammogram?
Most women age 40 to 74 can have a screening mammogram every 2 years. For those at higher risk for breast
cancer, screening should be considered as early as age 30.
For people who have or have not had Chest Construction Surgery, or who have breast (chest) tissue from
taking gender-affirming hormones, refer to the Screening Strategy Based on Anatomy Present section for
more information. Screening is also available for Two-Spirit, transgender or gender-diverse (TTGD) individuals.
Patient Characteristics Recommendation Referral
Average Risk
Age 39 and under Routine screening mammogram is not recommended (refer to High Risk
section below).
Age 40 to 49 Screening mammography
is available every 2 years.
Speak with the patient
about the benefits
and limitations of
mammography.
No referral required. Patient can call a
breast screening centre directly or 1-800-
663-9203 to book their appointment.
Inform the patient that they will
need to identify a health care
provider (physician, nurse
practitioner, naturopath or
walk-in clinic) who can followup
with them if needed.
Age 50 to 74 Routine screening
mammogram every 2
years.
Age 75 and over Screening mammography
is available every 2 years
if the patient is in good
general health. Speak
with the patient about the
benefits and limitations of
mammography.
Higher than Average Risk
Age 40 to 74
1st degree relative2 with
breast cancer
Routine screening
mammogram every year.
No referral required. Patient can call a
breast screening centre directly or 1-800-
663-9203 to book their appointment.
Inform the patient that they will
need to identify a health care
provider (physician, nurse
practitioner, naturopath or walkin
clinic) who can follow-up
with them if needed.
2 Parent, child, sibling
(continued on next page)
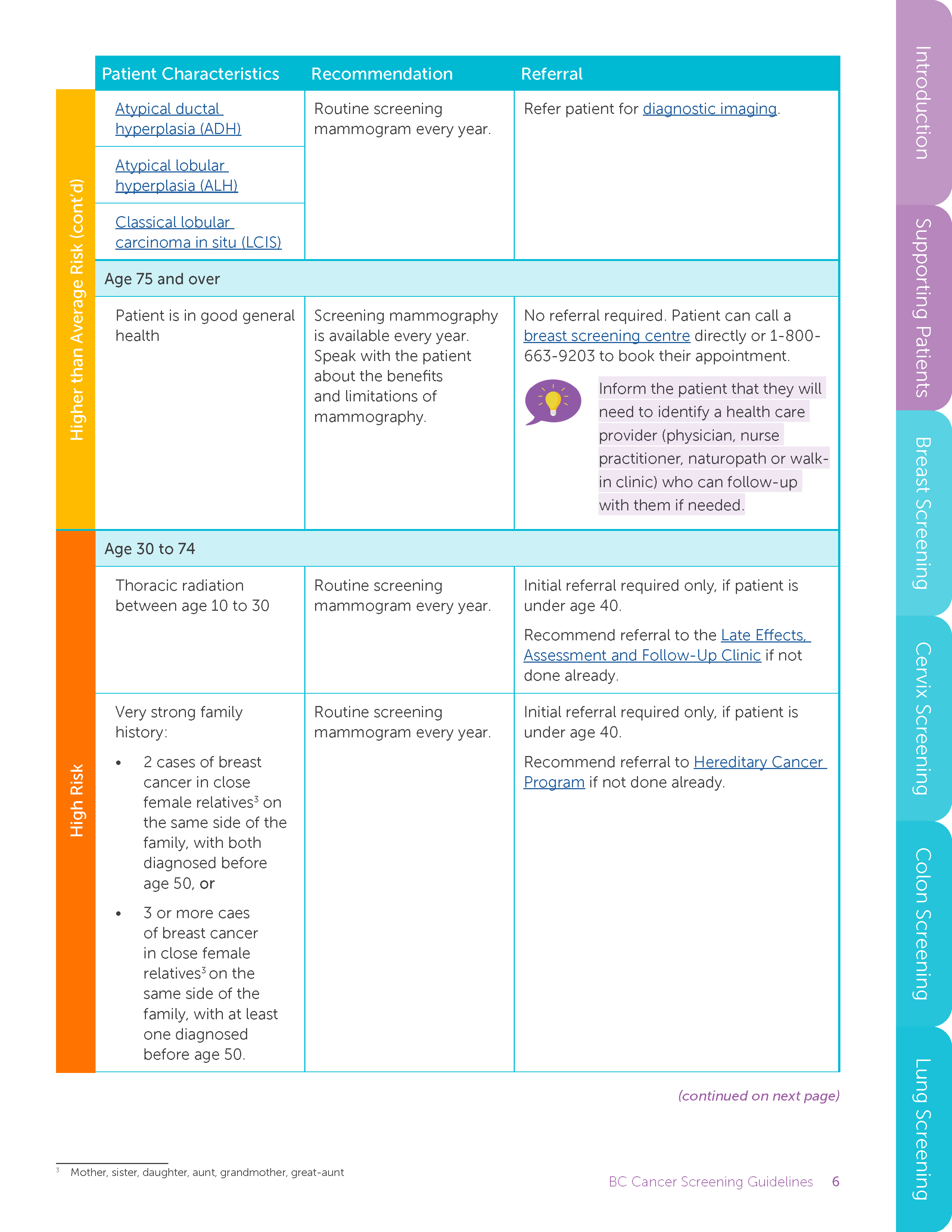
BC Cancer Screening Guidelines 6
Patient Characteristics Recommendation Referral
Higher than Average Risk (cont’d)
Atypical ductal
hyperplasia (ADH)
Routine screening
mammogram every year.
Refer patient for diagnostic imaging.
Atypical lobular
hyperplasia (ALH)
Classical lobular
carcinoma in situ (LCIS)
Age 75 and over
Patient is in good general
health
Screening mammography
is available every year.
Speak with the patient
about the benefits
and limitations of
mammography.
No referral required. Patient can call a
breast screening centre directly or 1-800-
663-9203 to book their appointment.
Inform the patient that they will
need to identify a health care
provider (physician, nurse
practitioner, naturopath or walkin
clinic) who can follow-up
with them if needed.
High Risk
Age 30 to 74
Thoracic radiation
between age 10 to 30
Routine screening
mammogram every year.
Initial referral required only, if patient is
under age 40.
Recommend referral to the Late Effects,
Assessment and Follow-Up Clinic if not
done already.
Very strong family
history:
• 2 cases of breast
cancer in close
female relatives3 on
the same side of the
family, with both
diagnosed before
age 50, or
• 3 or more caes
of breast cancer
in close female
relatives3 on the
same side of the
family, with at least
one diagnosed
before age 50.
Routine screening
mammogram every year.
Initial referral required only, if patient is
under age 40.
Recommend referral to Hereditary Cancer
Program if not done already.
3 Mother, sister, daughter, aunt, grandmother, great-aunt
(continued on next page)
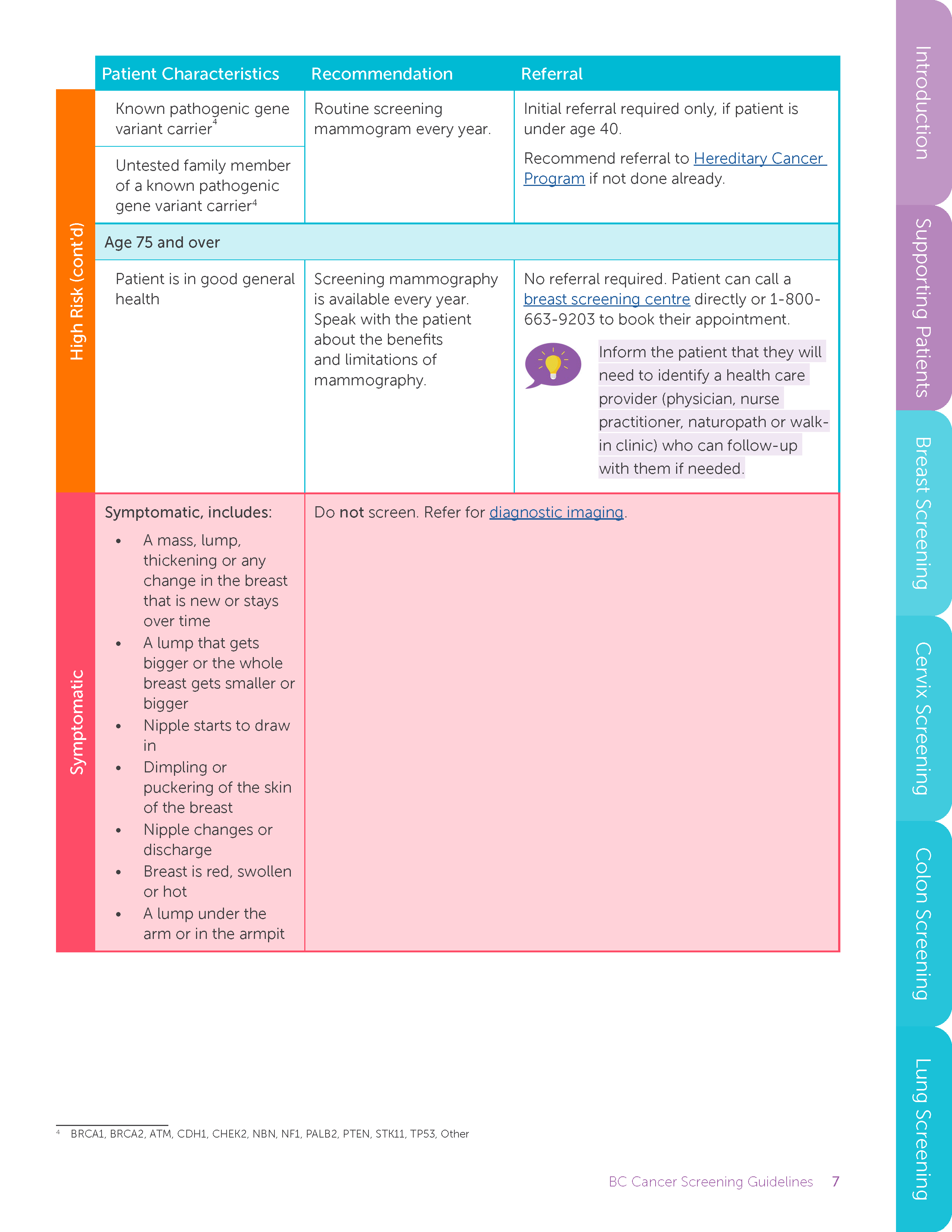
BC Cancer Screening Guidelines 7
Patient Characteristics Recommendation Referral
High Risk (cont'd)
Known pathogenic gene
variant carrier4
Routine screening
mammogram every year.
Initial referral required only, if patient is
under age 40.
Recommend referral to Hereditary Cancer
Program if not done already.
Untested family member
of a known pathogenic
gene variant carrier4
Age 75 and over
Patient is in good general
health
Screening mammography
is available every year.
Speak with the patient
about the benefits
and limitations of
mammography.
No referral required. Patient can call a
breast screening centre directly or 1-800-
663-9203 to book their appointment.
Inform the patient that they will
need to identify a health care
provider (physician, nurse
practitioner, naturopath or walkin
clinic) who can follow-up
with them if needed.
Symptomatic
Symptomatic, includes:
• A mass, lump,
thickening or any
change in the breast
that is new or stays
over time
• A lump that gets
bigger or the whole
breast gets smaller or
bigger
• Nipple starts to draw
in
• Dimpling or
puckering of the skin
of the breast
• Nipple changes or
discharge
• Breast is red, swollen
or hot
• A lump under the
arm or in the armpit
Do not screen. Refer for diagnostic imaging.
4 BRCA1, BRCA2, ATM, CDH1, CHEK2, NBN, NF1, PALB2, PTEN, STK11, TP53, Other
BC Cancer Screening Guidelines 8
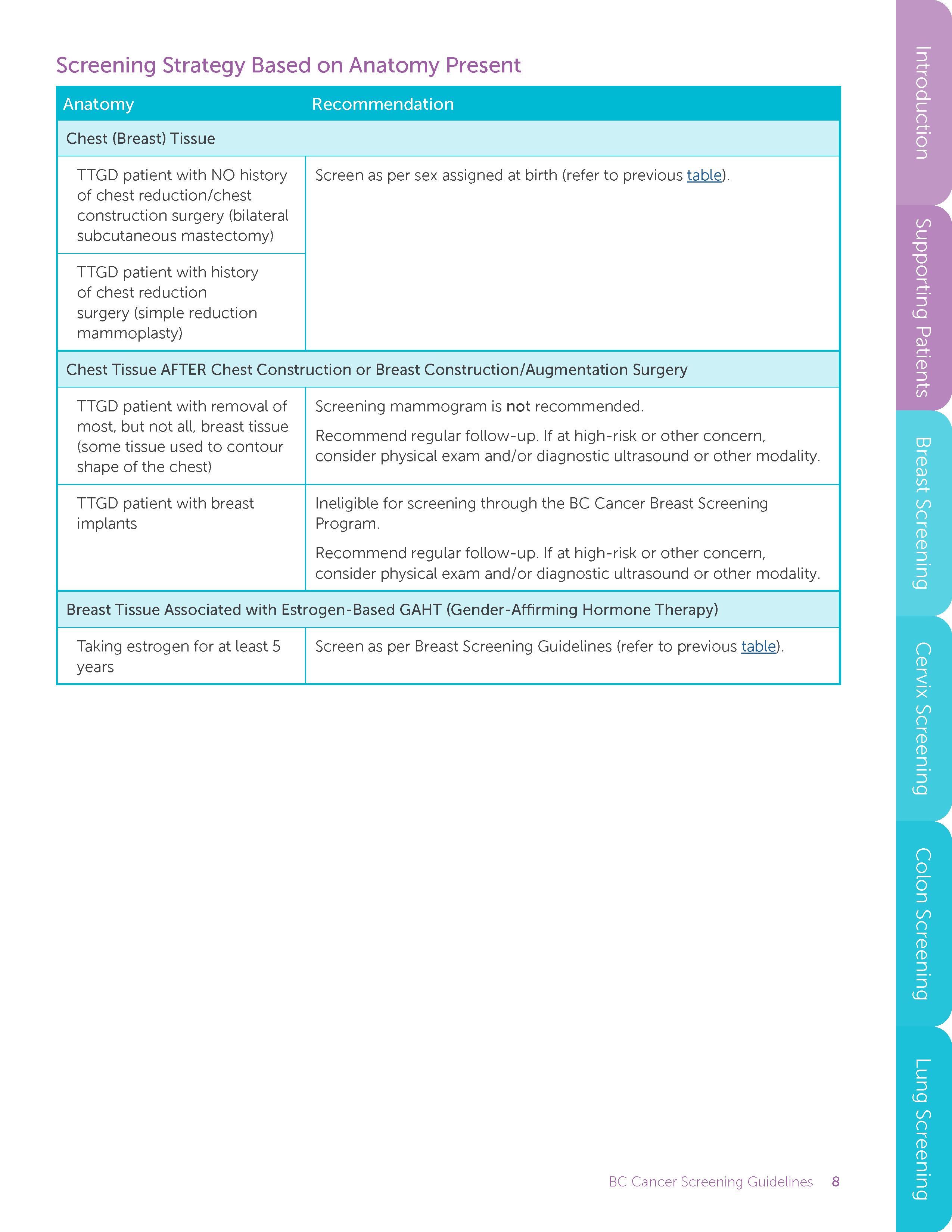
Screening Strategy Based on Anatomy Present
Anatomy Recommendation
Chest (Breast) Tissue
TTGD patient with NO history
of chest reduction/chest
construction surgery (bilateral
subcutaneous mastectomy)
Screen as per sex assigned at birth (refer to previous table).
TTGD patient with history
of chest reduction
surgery (simple reduction
mammoplasty)
Chest Tissue AFTER Chest Construction or Breast Construction/Augmentation Surgery
TTGD patient with removal of
most, but not all, breast tissue
(some tissue used to contour
shape of the chest)
Screening mammogram is not recommended.
Recommend regular follow-up. If at high-risk or other concern,
consider physical exam and/or diagnostic ultrasound or other modality.
TTGD patient with breast
implants
Ineligible for screening through the BC Cancer Breast Screening
Program.
Recommend regular follow-up. If at high-risk or other concern,
consider physical exam and/or diagnostic ultrasound or other modality.
Breast Tissue Associated with Estrogen-Based GAHT (Gender-Affirming Hormone Therapy)
Taking estrogen for at least 5
years
Screen as per Breast Screening Guidelines (refer to previous table).
BC Cancer Screening Guidelines 9
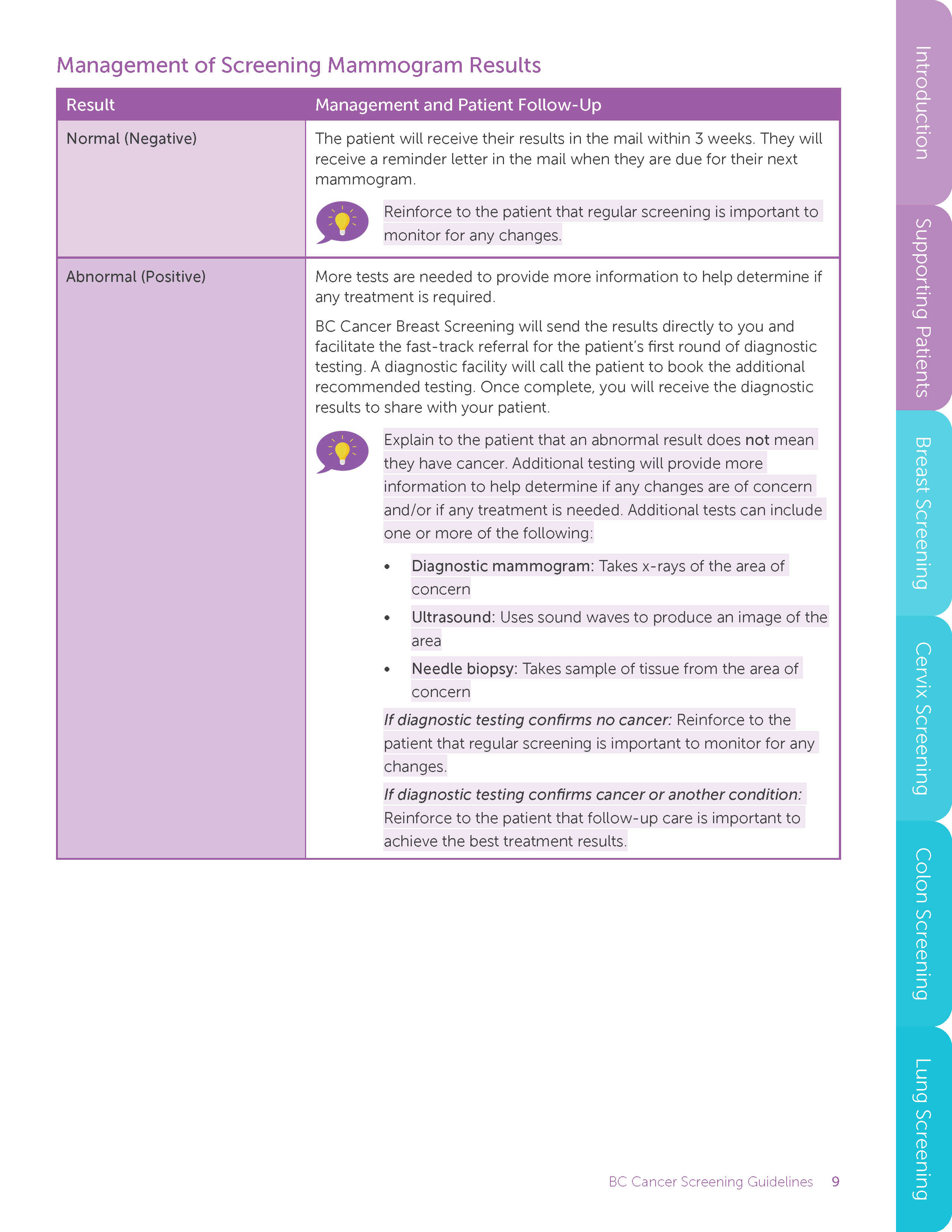
Management of Screening Mammogram Results
Result Management and Patient Follow-Up
Normal (Negative) The patient will receive their results in the mail within 3 weeks. They will
receive a reminder letter in the mail when they are due for their next
mammogram.
Reinforce to the patient that regular screening is important to
monitor for any changes.
Abnormal (Positive) More tests are needed to provide more information to help determine if
any treatment is required.
BC Cancer Breast Screening will send the results directly to you and
facilitate the fast-track referral for the patient’s first round of diagnostic
testing. A diagnostic facility will call the patient to book the additional
recommended testing. Once complete, you will receive the diagnostic
results to share with your patient.
Explain to the patient that an abnormal result does not mean
they have cancer. Additional testing will provide more
information to help determine if any changes are of concern
and/or if any treatment is needed. Additional tests can include
one or more of the following:
• Diagnostic mammogram: Takes x-rays of the area of
concern
• Ultrasound: Uses sound waves to produce an image of the
area
• Needle biopsy: Takes sample of tissue from the area of
concern
If diagnostic testing confirms no cancer: Reinforce to the
patient that regular screening is important to monitor for any
changes.
If diagnostic testing confirms cancer or another condition:
Reinforce to the patient that follow-up care is important to
achieve the best treatment results.
BC Cancer Screening Guidelines 10
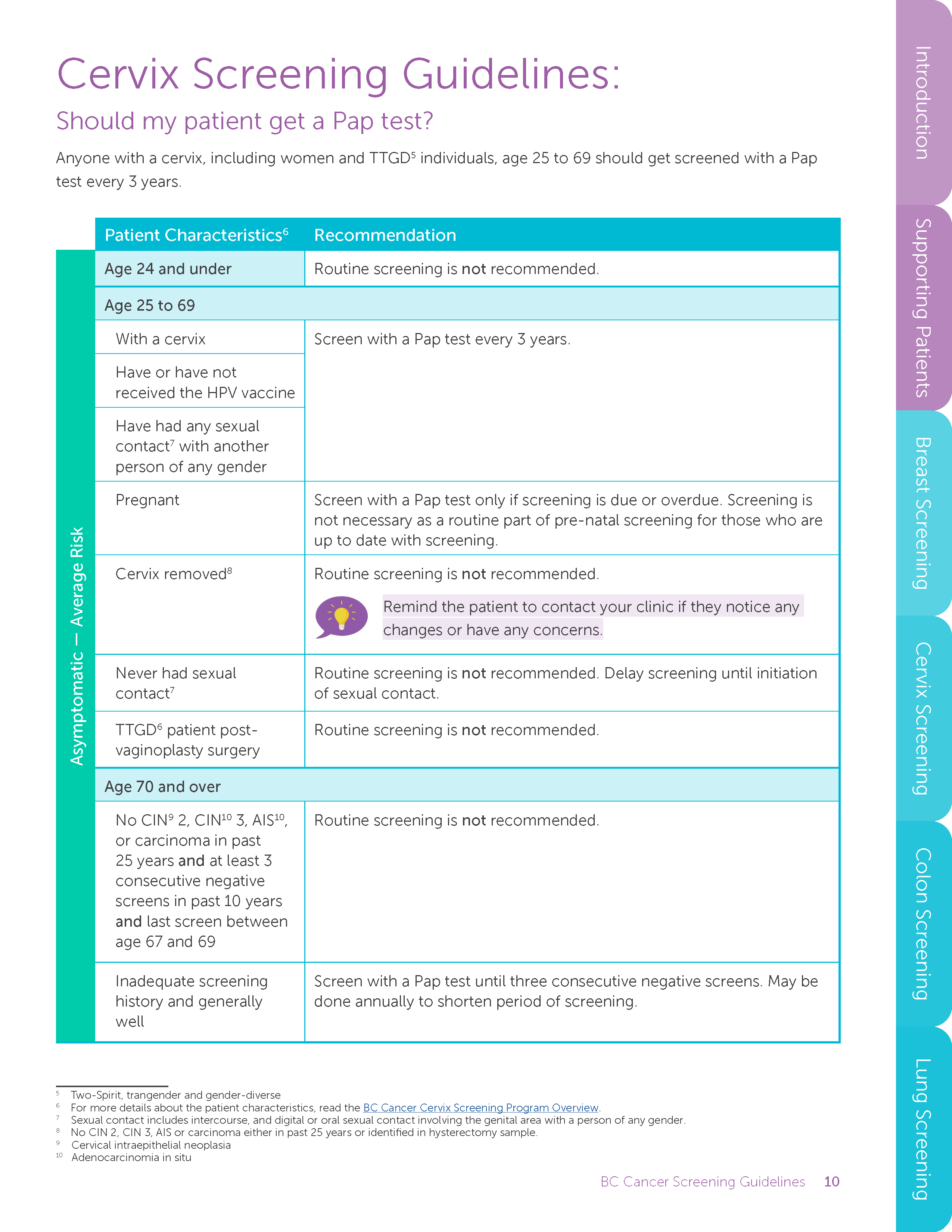
Cervix Screening Guidelines:
Should my patient get a Pap test?
Anyone with a cervix, including women and TTGD5 individuals, age 25 to 69 should get screened with a Pap
test every 3 years.
Patient Characteristics6 Recommendation
Asymptomatic — Average Risk
Age 24 and under Routine screening is not recommended.
Age 25 to 69
With a cervix Screen with a Pap test every 3 years.
Have or have not
received the HPV vaccine
Have had any sexual
contact7 with another
person of any gender
Pregnant Screen with a Pap test only if screening is due or overdue. Screening is
not necessary as a routine part of pre-natal screening for those who are
up to date with screening.
Cervix removed8 Routine screening is not recommended.
Remind the patient to contact your clinic if they notice any
changes or have any concerns.
Never had sexual
contact7
Routine screening is not recommended. Delay screening until initiation
of sexual contact.
TTGD6 patient postvaginoplasty
surgery
Routine screening is not recommended.
Age 70 and over
No CIN9 2, CIN10 3, AIS10,
or carcinoma in past
25 years and at least 3
consecutive negative
screens in past 10 years
and last screen between
age 67 and 69
Routine screening is not recommended.
Inadequate screening
history and generally
well
Screen with a Pap test until three consecutive negative screens. May be
done annually to shorten period of screening.
5 Two-Spirit, trangender and gender-diverse
6 For more details about the patient characteristics, read the BC Cancer Cervix Screening Program Overview.
7 Sexual contact includes intercourse, and digital or oral sexual contact involving the genital area with a person of any gender.
8 No CIN 2, CIN 3, AIS or carcinoma either in past 25 years or identified in hysterectomy sample.
9 Cervical intraepithelial neoplasia
10 Adenocarcinomia in situ
BC Cancer Screening Guidelines 11
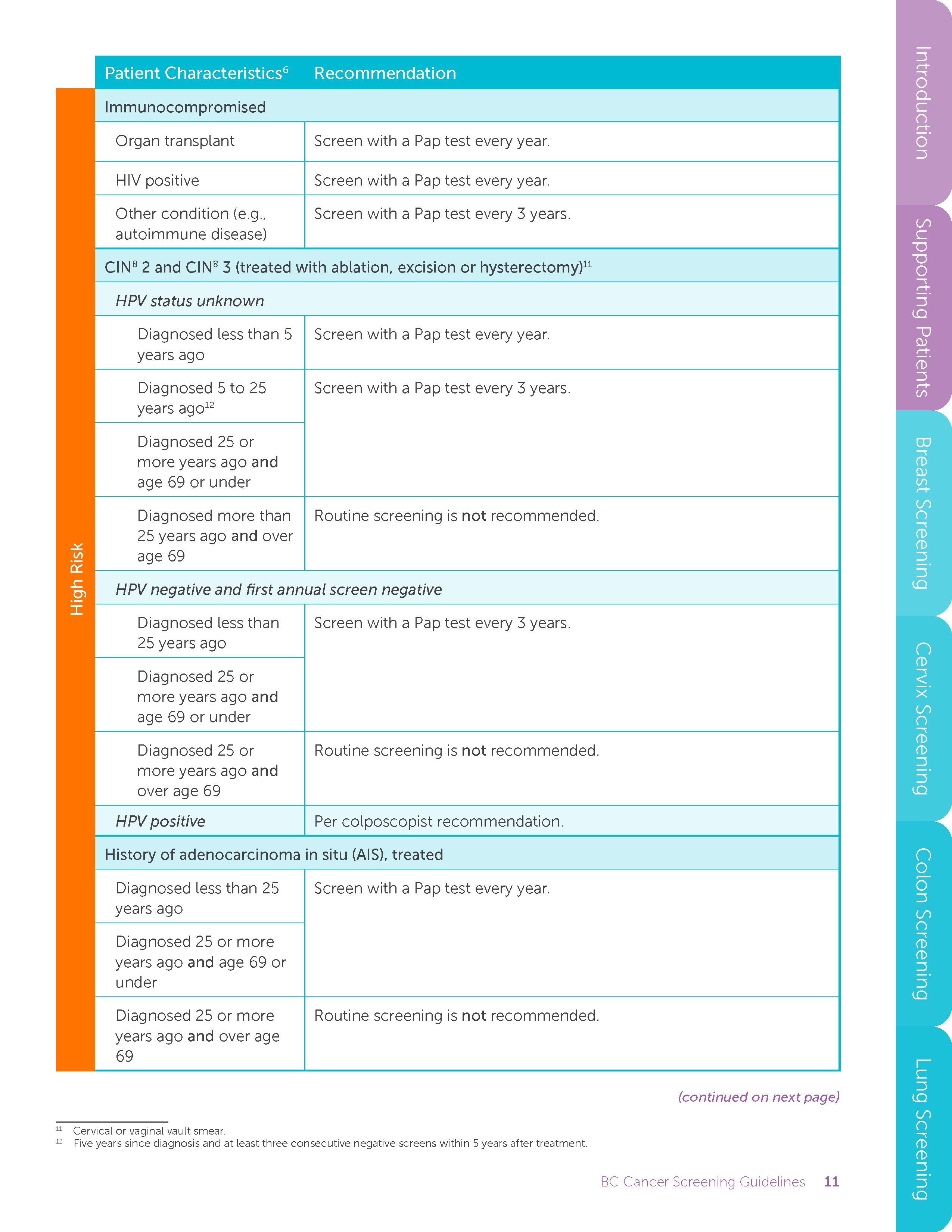
Patient Characteristics6 Recommendation
High Risk
Immunocompromised
Organ transplant Screen with a Pap test every year.
HIV positive Screen with a Pap test every year.
Other condition (e.g.,
autoimmune disease)
Screen with a Pap test every 3 years.
CIN8 2 and CIN8 3 (treated with ablation, excision or hysterectomy)11
HPV status unknown
Diagnosed less than 5
years ago
Screen with a Pap test every year.
Diagnosed 5 to 25
years ago12
Screen with a Pap test every 3 years.
Diagnosed 25 or
more years ago and
age 69 or under
Diagnosed more than
25 years ago and over
age 69
Routine screening is not recommended.
HPV negative and first annual screen negative
Diagnosed less than
25 years ago
Screen with a Pap test every 3 years.
Diagnosed 25 or
more years ago and
age 69 or under
Diagnosed 25 or
more years ago and
over age 69
Routine screening is not recommended.
HPV positive Per colposcopist recommendation.
History of adenocarcinoma in situ (AIS), treated
Diagnosed less than 25
years ago
Screen with a Pap test every year.
Diagnosed 25 or more
years ago and age 69 or
under
Diagnosed 25 or more
years ago and over age
69
Routine screening is not recommended.
11 Cervical or vaginal vault smear.
12 Five years since diagnosis and at least three consecutive negative screens within 5 years after treatment.
(continued on next page)
BC Cancer Screening Guidelines 12
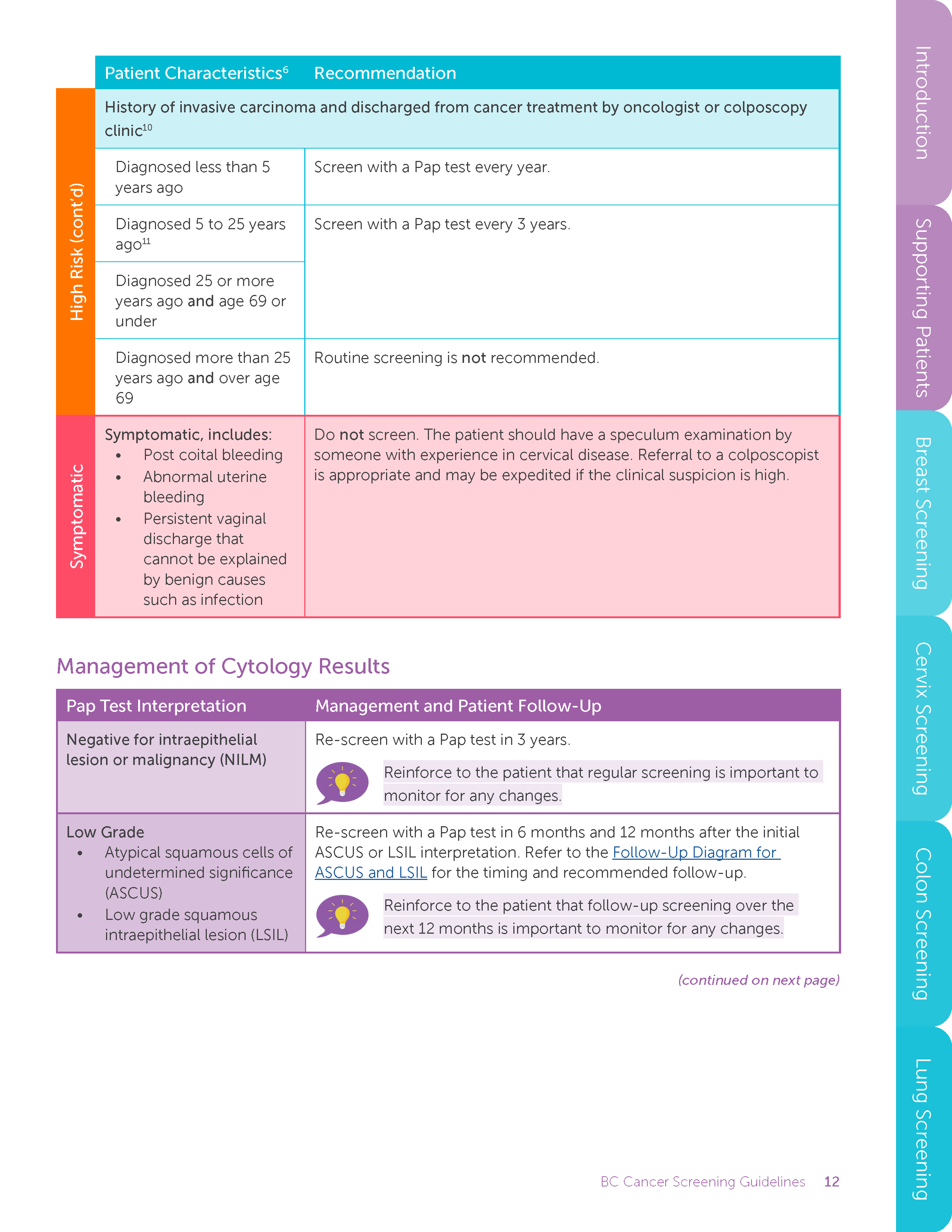
Patient Characteristics6 Recommendation
High Risk (cont’d)
History of invasive carcinoma and discharged from cancer treatment by oncologist or colposcopy
clinic10
Diagnosed less than 5
years ago
Screen with a Pap test every year.
Diagnosed 5 to 25 years
ago11
Screen with a Pap test every 3 years.
Diagnosed 25 or more
years ago and age 69 or
under
Diagnosed more than 25
years ago and over age
69
Routine screening is not recommended.
Symptomatic
Symptomatic, includes:
• Post coital bleeding
• Abnormal uterine
bleeding
• Persistent vaginal
discharge that
cannot be explained
by benign causes
such as infection
Do not screen. The patient should have a speculum examination by
someone with experience in cervical disease. Referral to a colposcopist
is appropriate and may be expedited if the clinical suspicion is high.
Management of Cytology Results
Pap Test Interpretation Management and Patient Follow-Up
Negative for intraepithelial
lesion or malignancy (NILM)
Re-screen with a Pap test in 3 years.
Reinforce to the patient that regular screening is important to
monitor for any changes.
Low Grade
• Atypical squamous cells of
undetermined significance
(ASCUS)
• Low grade squamous
intraepithelial lesion (LSIL)
Re-screen with a Pap test in 6 months and 12 months after the initial
ASCUS or LSIL interpretation. Refer to the Follow-Up Diagram for
ASCUS and LSIL for the timing and recommended follow-up.
Reinforce to the patient that follow-up screening over the
next 12 months is important to monitor for any changes.
(continued on next page)
BC Cancer Screening Guidelines 13
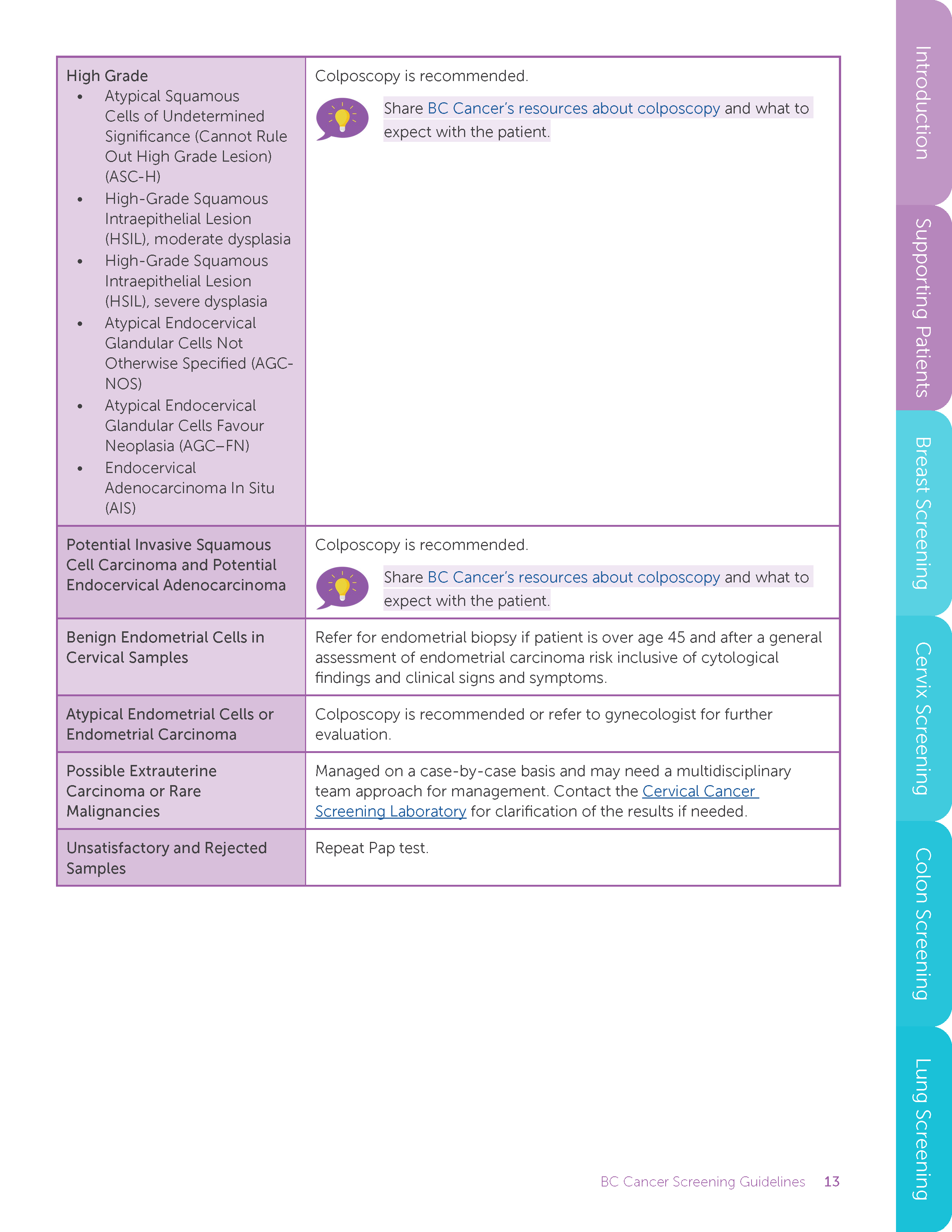
High Grade
• Atypical Squamous
Cells of Undetermined
Significance (Cannot Rule
Out High Grade Lesion)
(ASC-H)
• High-Grade Squamous
Intraepithelial Lesion
(HSIL), moderate dysplasia
• High-Grade Squamous
Intraepithelial Lesion
(HSIL), severe dysplasia
• Atypical Endocervical
Glandular Cells Not
Otherwise Specified (AGCNOS)
• Atypical Endocervical
Glandular Cells Favour
Neoplasia (AGC–FN)
• Endocervical
Adenocarcinoma In Situ
(AIS)
Colposcopy is recommended.
Share BC Cancer’s resources about colposcopy and what to
expect with the patient.
Potential Invasive Squamous
Cell Carcinoma and Potential
Endocervical Adenocarcinoma
Colposcopy is recommended.
Share BC Cancer’s resources about colposcopy and what to
expect with the patient.
Benign Endometrial Cells in
Cervical Samples
Refer for endometrial biopsy if patient is over age 45 and after a general
assessment of endometrial carcinoma risk inclusive of cytological
findings and clinical signs and symptoms.
Atypical Endometrial Cells or
Endometrial Carcinoma
Colposcopy is recommended or refer to gynecologist for further
evaluation.
Possible Extrauterine
Carcinoma or Rare
Malignancies
Managed on a case-by-case basis and may need a multidisciplinary
team approach for management. Contact the Cervical Cancer
Screening Laboratory for clarification of the results if needed.
Unsatisfactory and Rejected
Samples
Repeat Pap test.
BC Cancer Screening Guidelines 14
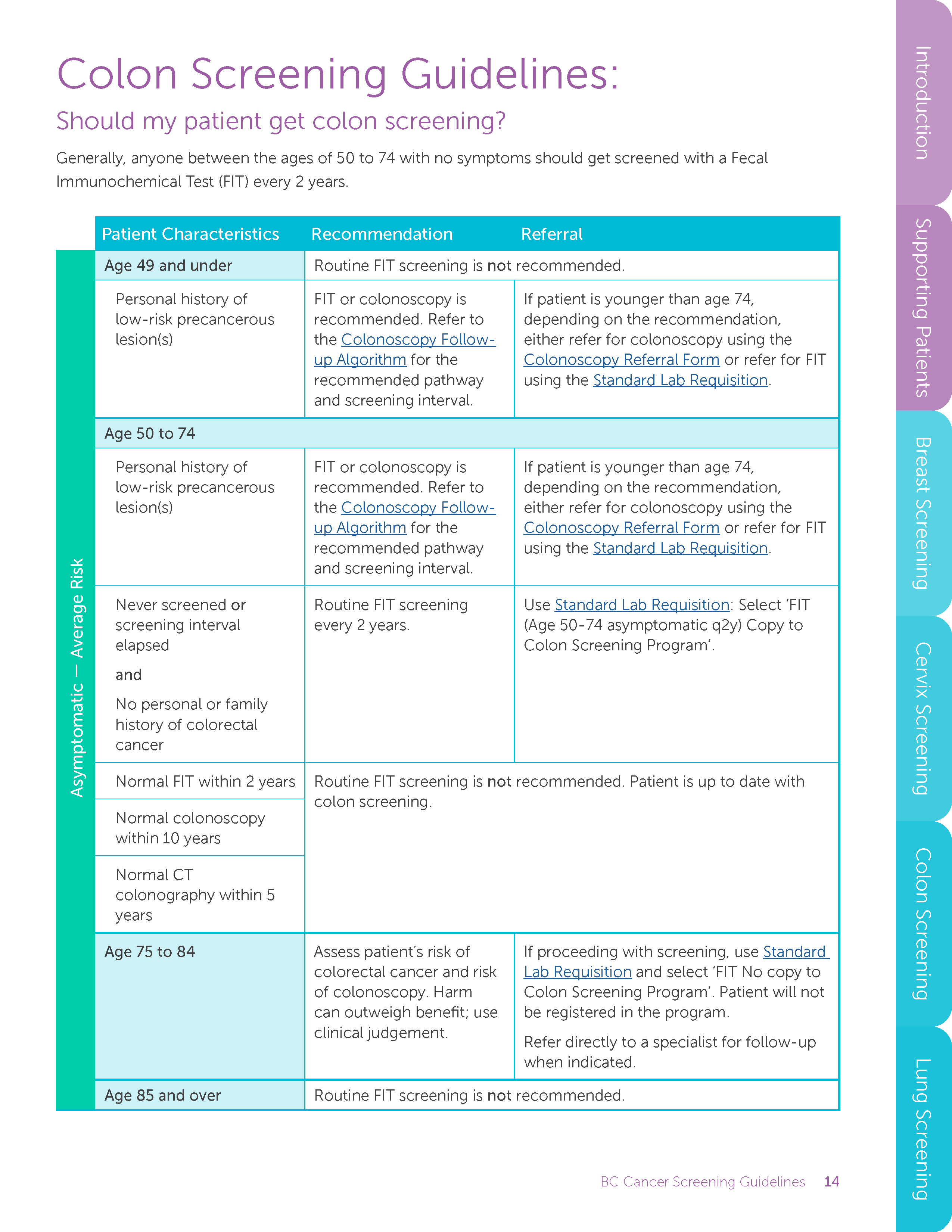
Colon Screening Guidelines:
Should my patient get colon screening?
Generally, anyone between the ages of 50 to 74 with no symptoms should get screened with a Fecal
Immunochemical Test (FIT) every 2 years.
Patient Characteristics Recommendation Referral
Asymptomatic — Average Risk
Age 49 and under Routine FIT screening is not recommended.
Personal history of
low-risk precancerous
lesion(s)
FIT or colonoscopy is
recommended. Refer to
the Colonoscopy Followup
Algorithm for the
recommended pathway
and screening interval.
If patient is younger than age 74,
depending on the recommendation,
either refer for colonoscopy using the
Colonoscopy Referral Form or refer for FIT
using the Standard Lab Requisition.
Age 50 to 74
Personal history of
low-risk precancerous
lesion(s)
FIT or colonoscopy is
recommended. Refer to
the Colonoscopy Followup
Algorithm for the
recommended pathway
and screening interval.
If patient is younger than age 74,
depending on the recommendation,
either refer for colonoscopy using the
Colonoscopy Referral Form or refer for FIT
using the Standard Lab Requisition.
Never screened or
screening interval
elapsed
and
No personal or family
history of colorectal
cancer
Routine FIT screening
every 2 years.
Use Standard Lab Requisition: Select ‘FIT
(Age 50-74 asymptomatic q2y) Copy to
Colon Screening Program’.
Normal FIT within 2 years Routine FIT screening is not recommended. Patient is up to date with
colon screening.
Normal colonoscopy
within 10 years
Normal CT
colonography within 5
years
Age 75 to 84 Assess patient’s risk of
colorectal cancer and risk
of colonoscopy. Harm
can outweigh benefit; use
clinical judgement.
If proceeding with screening, use Standard
Lab Requisition and select ‘FIT No copy to
Colon Screening Program’. Patient will not
be registered in the program.
Refer directly to a specialist for follow-up
when indicated.
Age 85 and over Routine FIT screening is not recommended.
BC Cancer Screening Guidelines 15
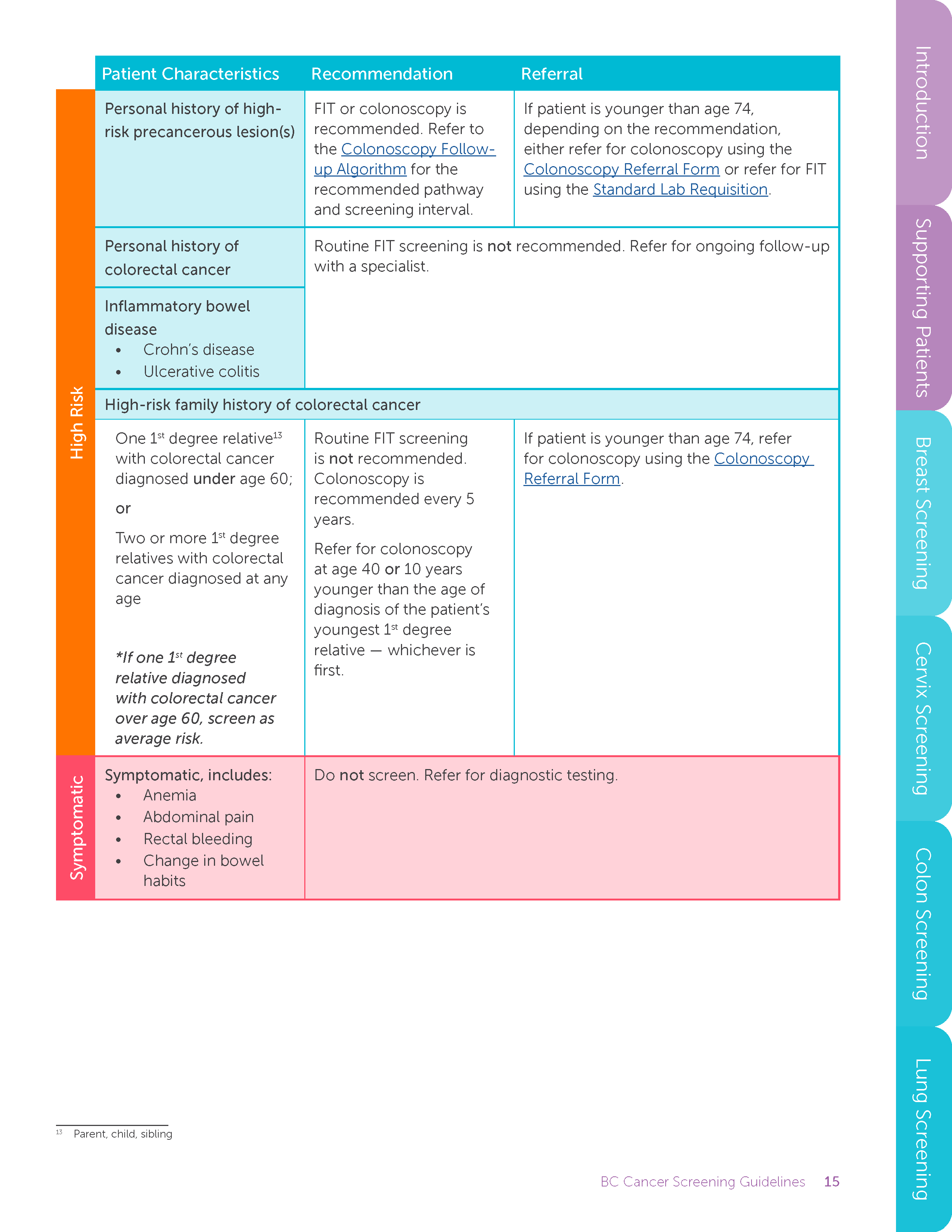
Patient Characteristics Recommendation Referral
High Risk
Personal history of highrisk
precancerous lesion(s)
FIT or colonoscopy is
recommended. Refer to
the Colonoscopy Followup
Algorithm for the
recommended pathway
and screening interval.
If patient is younger than age 74,
depending on the recommendation,
either refer for colonoscopy using the
Colonoscopy Referral Form or refer for FIT
using the Standard Lab Requisition.
Personal history of
colorectal cancer
Routine FIT screening is not recommended. Refer for ongoing follow-up
with a specialist.
Inflammatory bowel
disease
• Crohn’s disease
• Ulcerative colitis
High-risk family history of colorectal cancer
One 1st degree relative13
with colorectal cancer
diagnosed under age 60;
or
Two or more 1st degree
relatives with colorectal
cancer diagnosed at any
age
*If one 1st degree
relative diagnosed
with colorectal cancer
over age 60, screen as
average risk.
Routine FIT screening
is not recommended.
Colonoscopy is
recommended every 5
years.
Refer for colonoscopy
at age 40 or 10 years
younger than the age of
diagnosis of the patient’s
youngest 1st degree
relative — whichever is
first.
If patient is younger than age 74, refer
for colonoscopy using the Colonoscopy
Referral Form.
Symptomatic
Symptomatic, includes:
• Anemia
• Abdominal pain
• Rectal bleeding
• Change in bowel
habits
Do not screen. Refer for diagnostic testing.
13 Parent, child, sibling
BC Cancer Screening Guidelines 16
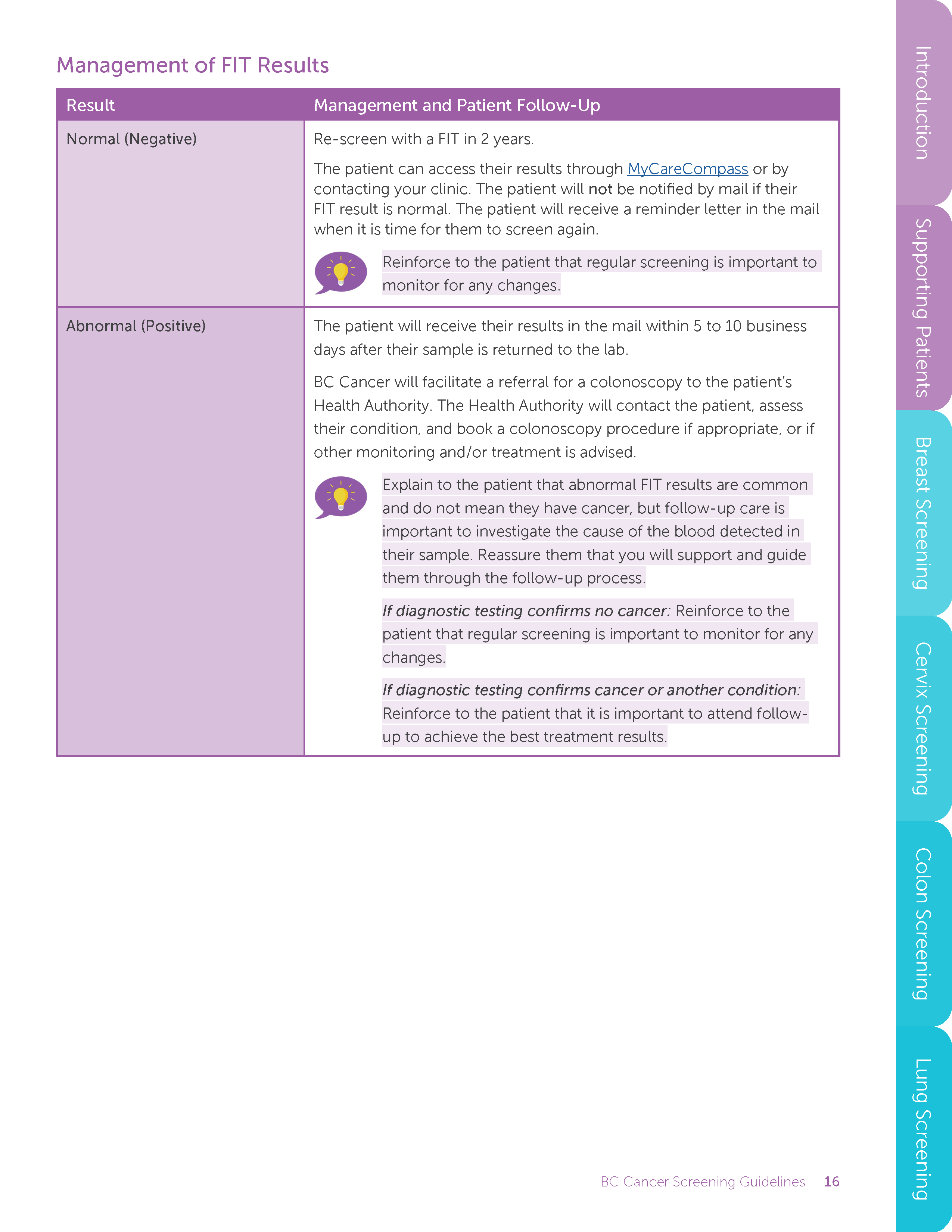
Management of FIT Results
Result Management and Patient Follow-Up
Normal (Negative) Re-screen with a FIT in 2 years.
The patient can access their results through MyCareCompass or by
contacting your clinic. The patient will not be notified by mail if their
FIT result is normal. The patient will receive a reminder letter in the mail
when it is time for them to screen again.
Reinforce to the patient that regular screening is important to
monitor for any changes.
Abnormal (Positive) The patient will receive their results in the mail within 5 to 10 business
days after their sample is returned to the lab.
BC Cancer will facilitate a referral for a colonoscopy to the patient’s
Health Authority. The Health Authority will contact the patient, assess
their condition, and book a colonoscopy procedure if appropriate, or if
other monitoring and/or treatment is advised.
Explain to the patient that abnormal FIT results are common
and do not mean they have cancer, but follow-up care is
important to investigate the cause of the blood detected in
their sample. Reassure them that you will support and guide
them through the follow-up process.
If diagnostic testing confirms no cancer: Reinforce to the
patient that regular screening is important to monitor for any
changes.
If diagnostic testing confirms cancer or another condition:
Reinforce to the patient that it is important to attend followup
to achieve the best treatment results.
BC Cancer Screening Guidelines 17
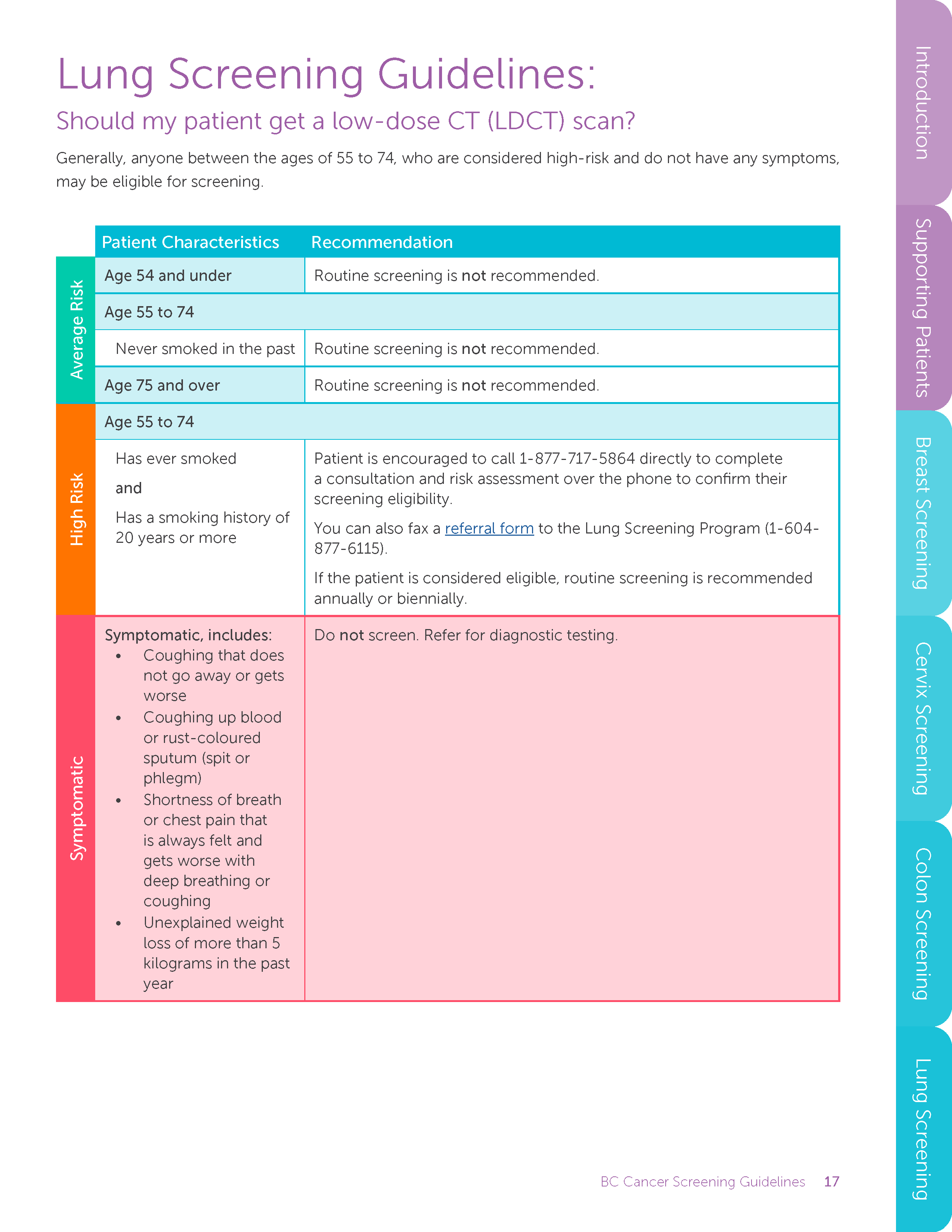
Lung Screening Guidelines:
Should my patient get a low-dose CT (LDCT) scan?
Generally, anyone between the ages of 55 to 74, who are considered high-risk and do not have any symptoms,
may be eligible for screening.
Patient Characteristics Recommendation
Average Risk
Age 54 and under Routine screening is not recommended.
Age 55 to 74
Never smoked in the past Routine screening is not recommended.
Age 75 and over Routine screening is not recommended.
High Risk
Age 55 to 74
Has ever smoked
and
Has a smoking history of
20 years or more
Patient is encouraged to call 1-877-717-5864 directly to complete
a consultation and risk assessment over the phone to confirm their
screening eligibility.
You can also fax a referral form to the Lung Screening Program (1-604-
877-6115).
If the patient is considered eligible, routine screening is recommended
annually or biennially.
Symptomatic
Symptomatic, includes:
• Coughing that does
not go away or gets
worse
• Coughing up blood
or rust-coloured
sputum (spit or
phlegm)
• Shortness of breath
or chest pain that
is always felt and
gets worse with
deep breathing or
coughing
• Unexplained weight
loss of more than 5
kilograms in the past
year
Do not screen. Refer for diagnostic testing.
BC Cancer Screening Guidelines 18
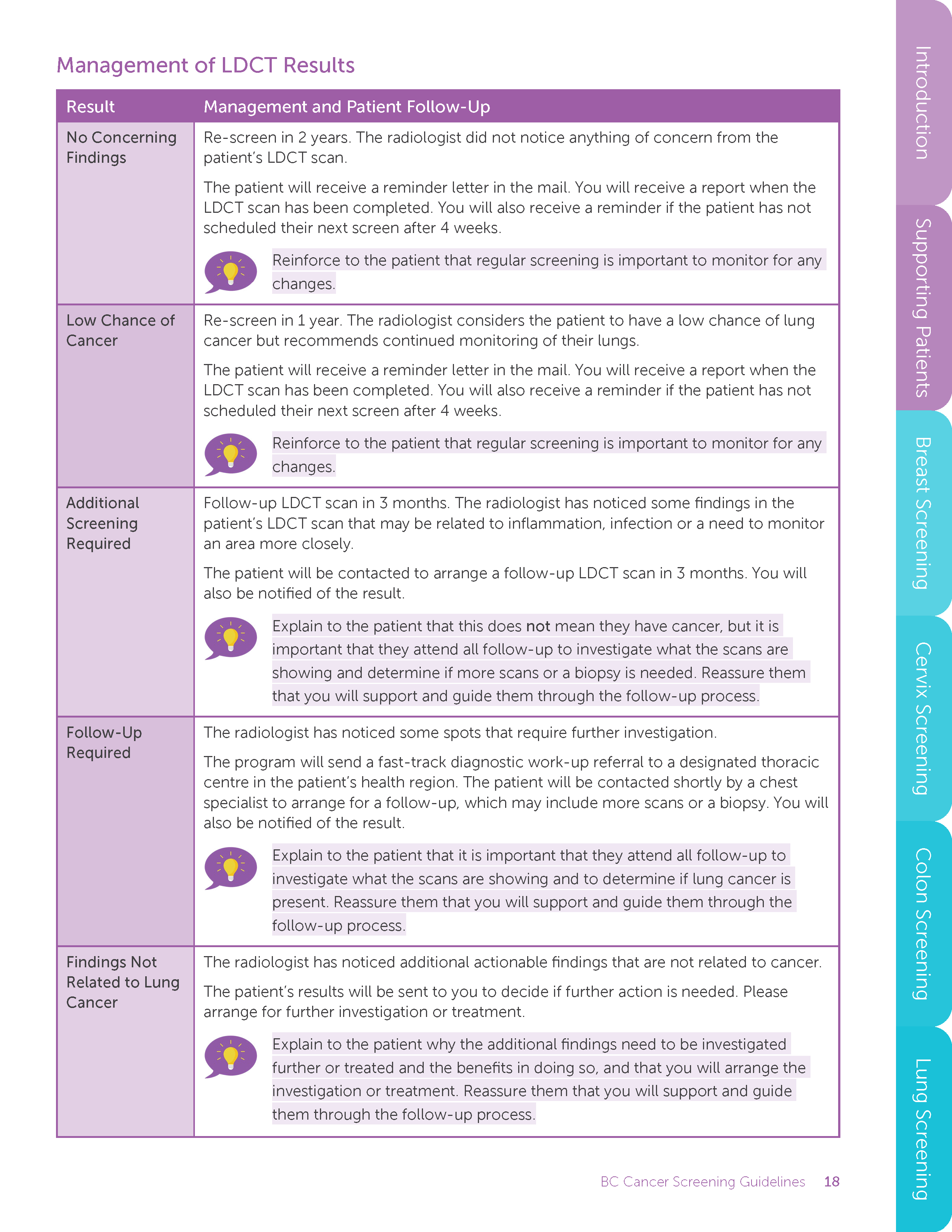
Management of LDCT Results
Result Management and Patient Follow-Up
No Concerning
Findings
Re-screen in 2 years. The radiologist did not notice anything of concern from the
patient’s LDCT scan.
The patient will receive a reminder letter in the mail. You will receive a report when the
LDCT scan has been completed. You will also receive a reminder if the patient has not
scheduled their next screen after 4 weeks.
Reinforce to the patient that regular screening is important to monitor for any
changes.
Low Chance of
Cancer
Re-screen in 1 year. The radiologist considers the patient to have a low chance of lung
cancer but recommends continued monitoring of their lungs.
The patient will receive a reminder letter in the mail. You will receive a report when the
LDCT scan has been completed. You will also receive a reminder if the patient has not
scheduled their next screen after 4 weeks.
Reinforce to the patient that regular screening is important to monitor for any
changes.
Additional
Screening
Required
Follow-up LDCT scan in 3 months. The radiologist has noticed some findings in the
patient’s LDCT scan that may be related to inflammation, infection or a need to monitor
an area more closely.
The patient will be contacted to arrange a follow-up LDCT scan in 3 months. You will
also be notified of the result.
Explain to the patient that this does not mean they have cancer, but it is
important that they attend all follow-up to investigate what the scans are
showing and determine if more scans or a biopsy is needed. Reassure them
that you will support and guide them through the follow-up process.
Follow-Up
Required
The radiologist has noticed some spots that require further investigation.
The program will send a fast-track diagnostic work-up referral to a designated thoracic
centre in the patient’s health region. The patient will be contacted shortly by a chest
specialist to arrange for a follow-up, which may include more scans or a biopsy. You will
also be notified of the result.
Explain to the patient that it is important that they attend all follow-up to
investigate what the scans are showing and to determine if lung cancer is
present. Reassure them that you will support and guide them through the
follow-up process.
Findings Not
Related to Lung
Cancer
The radiologist has noticed additional actionable findings that are not related to cancer.
The patient’s results will be sent to you to decide if further action is needed. Please
arrange for further investigation or treatment.
Explain to the patient why the additional findings need to be investigated
further or treated and the benefits in doing so, and that you will arrange the
investigation or treatment. Reassure them that you will support and guide
them through the follow-up process.
BC Cancer Screening Guidelines 19
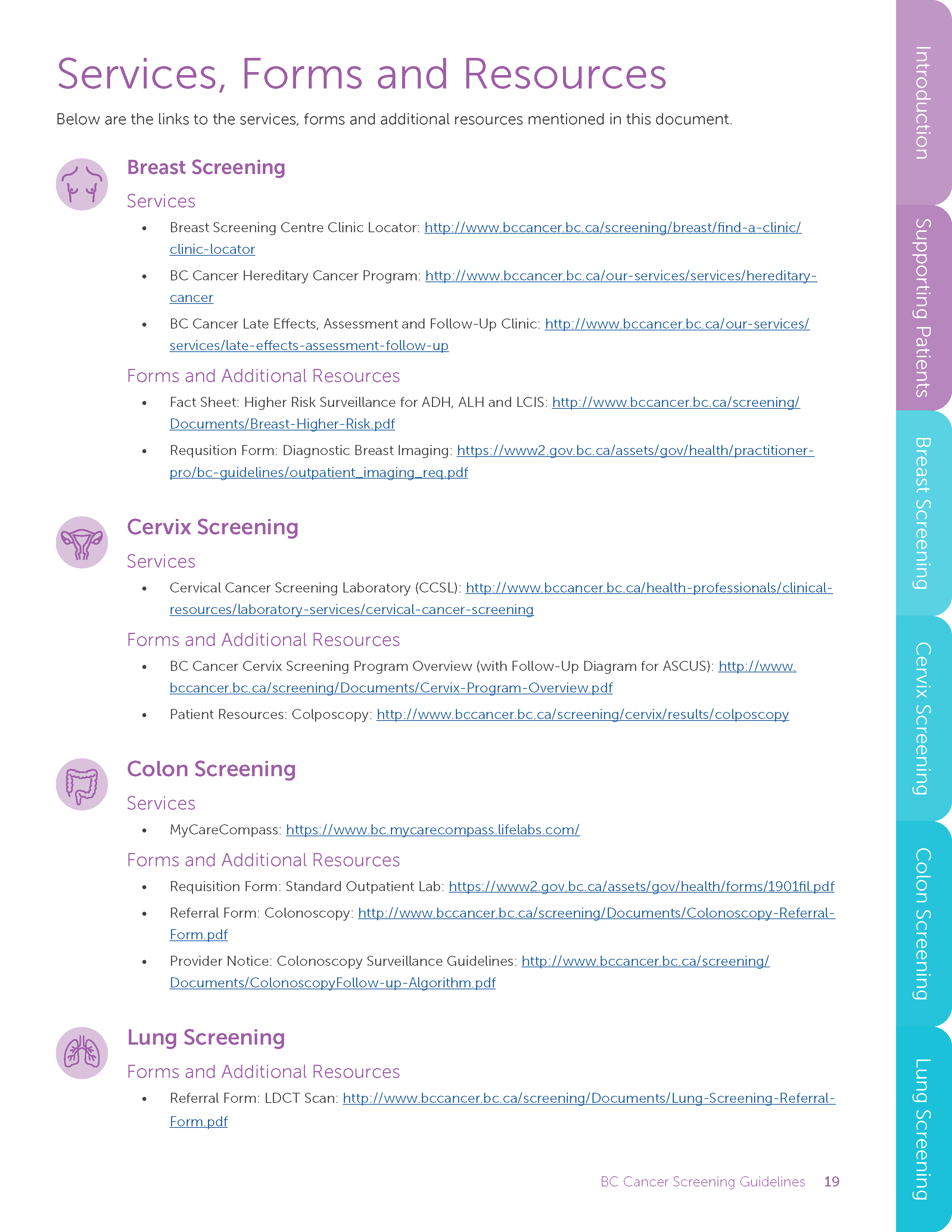
Services, Forms and Resources
Below are the links to the services, forms and additional resources mentioned in this document.
Breast Screening
Services
• Breast Screening Centre Clinic Locator: http://www.bccancer.bc.ca/screening/breast/find-a-clinic/
clinic-locator
• BC Cancer Hereditary Cancer Program: http://www.bccancer.bc.ca/our-services/services/hereditarycancer
• BC Cancer Late Effects, Assessment and Follow-Up Clinic: http://www.bccancer.bc.ca/our-services/
services/late-effects-assessment-follow-up
Forms and Additional Resources
• Fact Sheet: Higher Risk Surveillance for ADH, ALH and LCIS: http://www.bccancer.bc.ca/screening/
Documents/Breast-Higher-Risk.pdf
• Requsition Form: Diagnostic Breast Imaging: https://www2.gov.bc.ca/assets/gov/health/practitionerpro/
bc-guidelines/outpatient_imaging_req.pdf
Cervix Screening
Services
• Cervical Cancer Screening Laboratory (CCSL): http://www.bccancer.bc.ca/health-professionals/clinicalresources/
laboratory-services/cervical-cancer-screening
Forms and Additional Resources
• BC Cancer Cervix Screening Program Overview (with Follow-Up Diagram for ASCUS): http://www.
bccancer.bc.ca/screening/Documents/Cervix-Program-Overview.pdf
• Patient Resources: Colposcopy: http://www.bccancer.bc.ca/screening/cervix/results/colposcopy
Colon Screening
Services
• MyCareCompass: https://www.bc.mycarecompass.lifelabs.com/
Forms and Additional Resources
• Requisition Form: Standard Outpatient Lab: https://www2.gov.bc.ca/assets/gov/health/forms/1901fil.pdf
• Referral Form: Colonoscopy: http://www.bccancer.bc.ca/screening/Documents/Colonoscopy-Referral-
Form.pdf
• Provider Notice: Colonoscopy Surveillance Guidelines: http://www.bccancer.bc.ca/screening/
Documents/ColonoscopyFollow-up-Algorithm.pdf
Lung Screening
Forms and Additional Resources
• Referral Form: LDCT Scan: http://www.bccancer.bc.ca/screening/Documents/Lung-Screening-Referral-
Form.pdf