Source: Academic Life in Emergency Medicine
Gaze-Evoked Nystagmus
From: http://www.medscape.com/viewarticle/422863_3
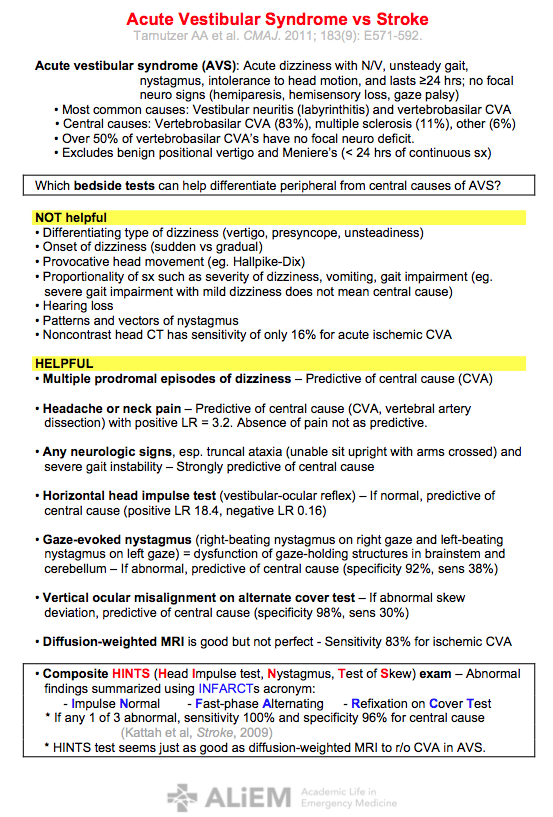
Action. Ask the patient to gaze at a target placed 20 to 30 degrees to the left and right of center for 20 seconds. Observe for gaze-evoked nystagmus or change in direction, form, or intensity in spontaneous nystagmus.
Interpretation. The ability to maintain eccentric gaze is under control of the brain stem and midline cerebellum, particularly the vestibulocerebellum (especially the flocculonodular lobes). When these mechanisms fail to hold the eye in the eccentric position, the eye drifts toward the midline (exponentially decreasing velocity), followed by refixation saccades toward the target. Such gaze-evoked nystagmus is central in origin and always beats in the direction of intended gaze. In contrast, enhancement of peripheral spontaneous nystagmus (linear slow component velocity) occurs without direction change when gazing in the direction of the fast phase. Causes of gaze-evoked nystagmus include a drug effect (sedatives, antiepileptics), alcohol, CNS tumors, and cerebellar degenerative syndromes.
Head Impulse Test
From: http://www.medscape.com/viewarticle/422863_3
Action. Ask the patient to fixate on a target on the wall in front of the patient while the examiner moves the patient's head rapidly (>2000 deg/sec2) to each side. The examiner looks for any movement of the pupil during the head thrust and a refixation saccade back to the target (Fig. 2). Either direct observation of pupillary movement or the use of an ophthalmoscope is employed to document eye movement.
Interpretation. Introduced by Halmagyi and Curthoys[5] in 1988, the head impulse test was described as a reliable sign of reduced vestibular function in the plane of rotation for the ear ipsilateral to the head thrust. The observation of eye movement during the maneuver is a sign of decreased neural input from the ipsilateral ear to the vestibulo-ocular reflex (VOR) because the contralateral ear is in inhibitory "saturation" and cannot supply enough neural activity to stabilize gaze. In such instances, the eye travels with the head during the high-velocity movement, and a refixation saccade is necessary to refoveate the target. Bilateral refixation movements are seen frequently in cases of ototoxicity.
Alternate Cover Test
From: http://www.fpnotebook.com/eye/exam/CvrTst.htm
- Child fixates on a point (e.g. small toy, penlight)
- Cover one eye for 1-2 seconds
- Rapidly uncover the first eye and cover the second for 1-2 seconds
- Rapidly uncover the second eye and cover the first again for 1-2 seconds
- Observe for refixation (suggests hidden phoria)
