** UPDATE: See SCAT5 **
Source: Concussion in Sport Group (group of international experts)
See also: Child-SCAT3 (for 5-12 yo)
Only 26.5% of Sport-Related Concussion (SRC) patients present to the ED, and of those only 10-20% will have delayed symptom resolution.
Notes regarding in-office management:
Have patient complete self-report section of SCAT3 or Child-SCAT3 prior to initial, and weekly follow-up visits.
Refer to sports medicine specialist if improvement not seen within 3 weeks.
Return to Learn (RTL) resource for patients and caregivers: http://www.nationwidechildrens.org/concussions-in-the-classroom
Return to Play (RTP) resource for patients and caregivers: http://www.parachutecanada.org/thinkfirstcanada
Full-text for indexing:
SCAT3 Sport ConCuSSion ASSeSment tool 3 | PAge 1 © 2013 Concussion in Sport Group
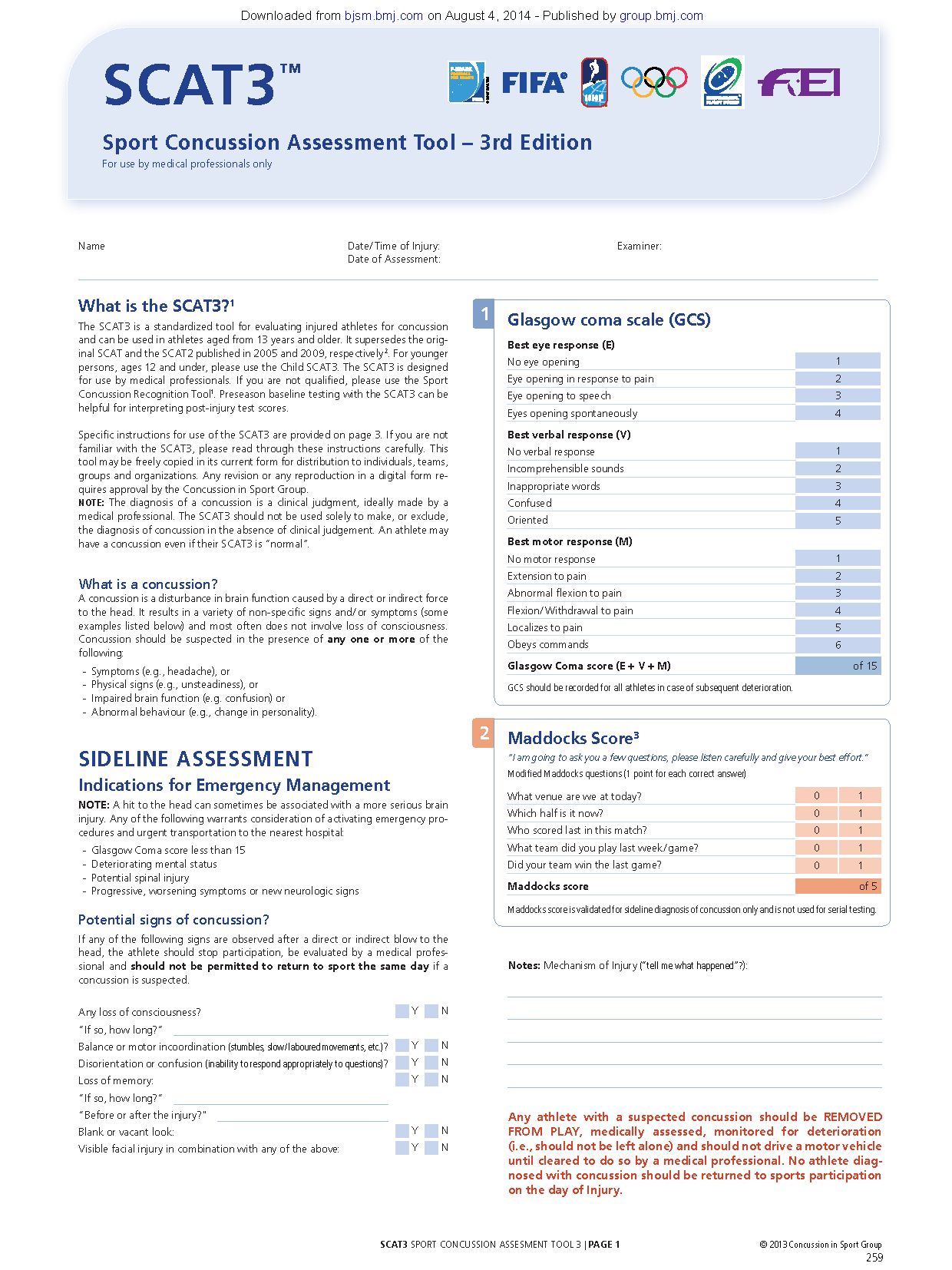
What is the SCAT3?1
the SCAt3 is a standardized tool for evaluating injured athletes for concussion
and can be used in athletes aged from 13 years and older. it supersedes the original
SCAt and the SCAt2 published in 2005 and 2009, respectively 2. For younger
persons, ages 12 and under, please use the Child SCAt3. the SCAt3 is designed
for use by medical professionals. If you are not qualifi ed, please use the Sport
Concussion recognition tool1. preseason baseline testing with the SCAt3 can be
helpful for interpreting post-injury test scores.
Specifi c instructions for use of the SCAT3 are provided on page 3. If you are not
familiar with the SCAt3, please read through these instructions carefully. this
tool may be freely copied in its current form for distribution to individuals, teams,
groups and organizations. Any revision or any reproduction in a digital form requires
approval by the Concussion in Sport Group.
NOTE: the diagnosis of a concussion is a clinical judgment, ideally made by a
medical professional. the SCAt3 should not be used solely to make, or exclude,
the diagnosis of concussion in the absence of clinical judgement. An athlete may
have a concussion even if their SCAt3 is “normal”.
What is a concussion?
A concussion is a disturbance in brain function caused by a direct or indirect force
to the head. It results in a variety of non-specifi c signs and / or symptoms (some
examples listed below) and most often does not involve loss of consciousness.
Concussion should be suspected in the presence of any one or more of the
following :
- Symptoms (e.g., headache), or
- Physical signs (e.g., unsteadiness), or
- Impaired brain function (e.g. confusion) or
- Abnormal behaviour (e.g., change in personality).
Sideline ASSeSSmenT
indications for emergency management
noTe: A hit to the head can sometimes be associated with a more serious brain
injury. Any of the following warrants consideration of activating emergency procedures
and urgent transportation to the nearest hospital:
- Glasgow Coma score less than 15
- Deteriorating mental status
- potential spinal injury
- progressive, worsening symptoms or new neurologic signs
P otential signs of concussion?
if any of the following signs are observed after a direct or indirect blow to the
head, the athlete should stop participation, be evaluated by a medical professional
and should not be permitted to return to sport the same day if a
concussion is suspected.
Any loss of consciousness? Y n
“if so, how long?“
Balance or motor incoordination (stumbles, slow / laboured movements, etc.)? Y n
Disorientation or confusion (inability to respond appropriately to questions)? Y n
loss of memory: Y n
“if so, how long?“
“Before or after the injury?"
Blank or vacant look: Y n
Visible facial injury in combination with any of the above: Y n
SCAT3™
Sport Concussion Assessment Tool – 3rd edition
For use by medical professionals only
glasgow coma scale (gCS)
Best eye response (e)
no eye opening 1
eye opening in response to pain 2
eye opening to speech 3
eyes opening spontaneously 4
Best verbal response (v)
no verbal response 1
incomprehensible sounds 2
inappropriate words 3
Confused 4
oriented 5
Best motor response (m)
no motor response 1
extension to pain 2
Abnormal fl exion to pain 3
Flexion / Withdrawal to pain 4
localizes to pain 5
obeys commands 6
glasgow Coma score (e + v + m) of 15
GCS should be recorded for all athletes in case of subsequent deterioration.
1
name Date / Time of Injury:
Date of Assessment:
examiner:
notes: mechanism of injury (“tell me what happened”?):
Any athlete with a suspected concussion should be removed
From PlAy, medically assessed, monitored for deterioration
(i.e., should not be left alone) and should not drive a motor vehicle
until cleared to do so by a medical professional. no athlete diagnosed
with concussion should be returned to sports participation
on the day of injury.
2 maddocks Score3
“I am going to ask you a few questions, please listen carefully and give your best effort.”
Modifi ed Maddocks questions (1 point for each correct answer)
What venue are we at today? 0 1
Which half is it now? 0 1
Who scored last in this match? 0 1
What team did you play last week / game? 0 1
Did your team win the last game? 0 1
maddocks score of 5
Maddocks score is validated for sideline diagnosis of concussion only and is not used for serial testing.
259
Downloaded from bjsm.bmj.com on August 4, 2014 - Published by group.bmj.com
SCAT3 Sport Concuss ion Ass esment Tool 3 | Page 2 © 2013 Concussion in Sport Group
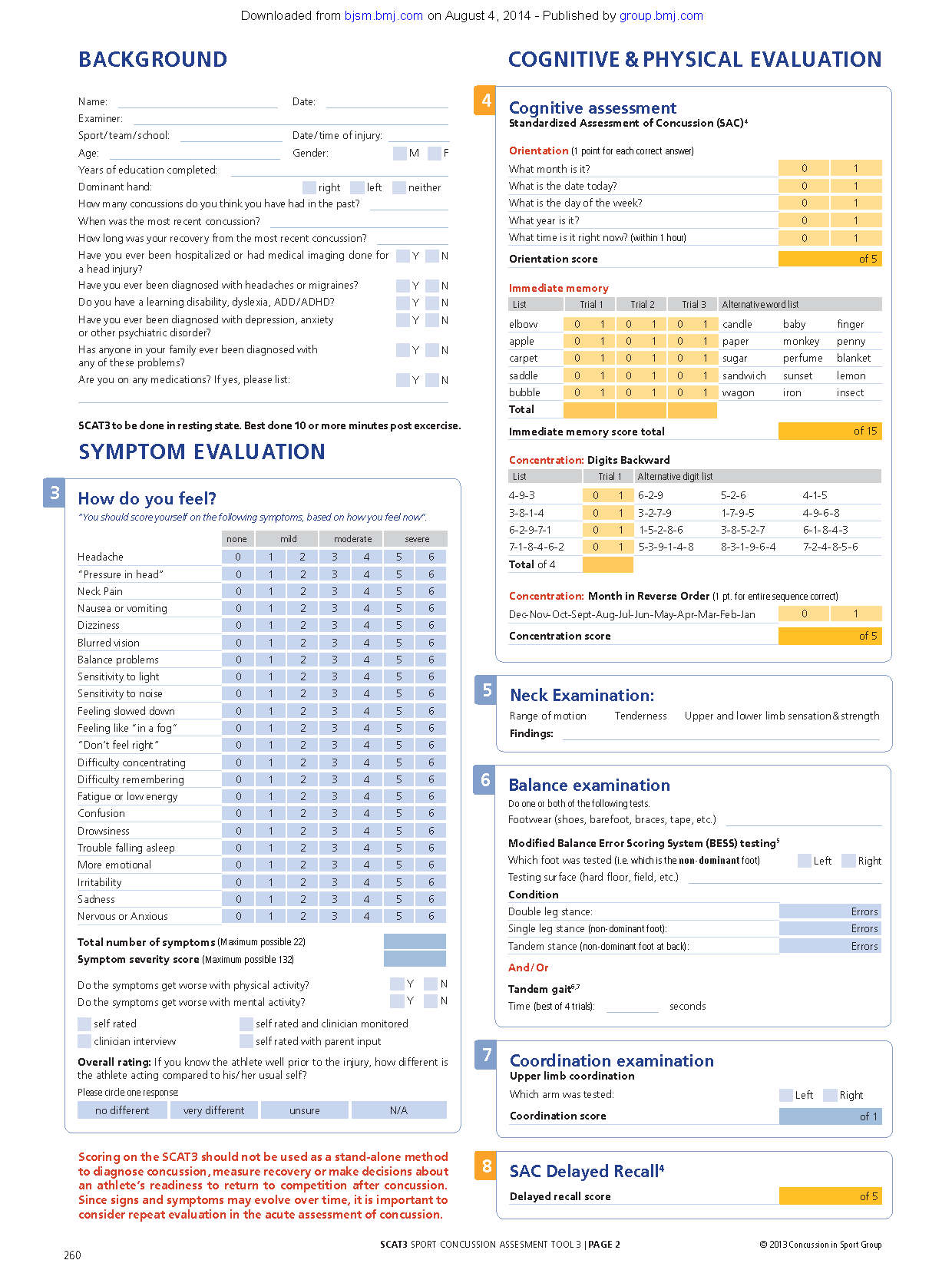
Cognitive & Physical Evaluat Background ion
Name: Date:
Examiner:
Sport / team / school: Date / time of injury:
Age: Gender: M F
Years of education completed:
Dominant hand: right left neither
How many concussions do you think you have had in the past?
When was the most recent concussion?
How long was your recovery from the most recent concussion?
Have you ever been hospitalized or had medical imaging done for
a head injury?
Y N
Have you ever been diagnosed with headaches or migraines? Y N
Do you have a learning disability, dyslexia, ADD / ADHD? Y N
Have you ever been diagnosed with depression, anxiety
or other psychiatric disorder?
Y N
Has anyone in your family ever been diagnosed with
any of these problems?
Y N
Are you on any medications? If yes, please list: Y N
SCAT3 to be done in resting state. Best done 10 or more minutes post excercise.
Symptom Evaluat ion
3 How do you feel?
“You should score yourself on the following symptoms, based on how you feel now”.
none mild moderate severe
Headache 0 1 2 3 4 5 6
“Pressure in head” 0 1 2 3 4 5 6
Neck Pain 0 1 2 3 4 5 6
Nausea or vomiting 0 1 2 3 4 5 6
Dizziness 0 1 2 3 4 5 6
Blurred vision 0 1 2 3 4 5 6
Balance problems 0 1 2 3 4 5 6
Sensitivity to light 0 1 2 3 4 5 6
Sensitivity to noise 0 1 2 3 4 5 6
Feeling slowed down 0 1 2 3 4 5 6
Feeling like “in a fog“ 0 1 2 3 4 5 6
“Don’t feel right” 0 1 2 3 4 5 6
Difficulty concentrating 0 1 2 3 4 5 6
Difficulty remembering 0 1 2 3 4 5 6
Fatigue or low energy 0 1 2 3 4 5 6
Confusion 0 1 2 3 4 5 6
Drowsiness 0 1 2 3 4 5 6
Trouble falling asleep 0 1 2 3 4 5 6
More emotional 0 1 2 3 4 5 6
Irritability 0 1 2 3 4 5 6
Sadness 0 1 2 3 4 5 6
Nervous or Anxious 0 1 2 3 4 5 6
Total number of symptoms (Maximum possible 22)
Symptom severity score (Maximum possible 132)
Do the symptoms get worse with physical activity? Y N
Do the symptoms get worse with mental activity? Y N
self rated self rated and clinician monitored
clinician interview self rated with parent input
Overall rating: If you know the athlete well prior to the injury, how different is
the athlete acting compared to his / her usual self?
Please circle one response:
no different very different unsure N/A
4 Cognitive assessment
Standardized Assessment of Concussion (SAC) 4
Orientation (1 point for each correct answer)
What month is it? 0 1
What is the date today? 0 1
What is the day of the week? 0 1
What year is it? 0 1
What time is it right now? (within 1 hour) 0 1
Orientation score of 5
Immediate memory
List Trial 1 Trial 2 Trial 3 Alternative word list
elbow 0 1 0 1 0 1 candle baby finger
apple 0 1 0 1 0 1 paper monkey penny
carpet 0 1 0 1 0 1 sugar perfume blanket
saddle 0 1 0 1 0 1 sandwich sunset lemon
bubble 0 1 0 1 0 1 wagon iron insect
Total
Immediate memory score total of 15
Concentration: Digits Backward
List Trial 1 Alternative digit list
4-9-3 0 1 6-2-9 5-2-6 4-1-5
3-8-1-4 0 1 3-2-7-9 1-7-9-5 4-9-6-8
6-2-9-7-1 0 1 1-5-2-8-6 3-8-5-2-7 6-1-8-4-3
7-1-8-4-6-2 0 1 5-3-9-1-4-8 8-3-1-9-6-4 7-2-4-8-5-6
Total of 4
Concentration: Month in Reverse Order (1 pt. for entire sequence correct)
Dec-Nov-Oct-Sept-Aug-Jul-Jun-May-Apr-Mar-Feb-Jan 0 1
Concentration score of 5
8 SAC Delayed Recall4
Delayed recall score of 5
Balance examination
Do one or both of the following tests.
Footwear (shoes, barefoot, braces, tape, etc.)
Modified Balance Error Scoring System (BESS) testing5
Which foot was tested (i.e. which is the non-dominant foot) Left Right
Testing surface (hard floor, field, etc.)
Condition
Double leg stance: Errors
Single leg stance (non-dominant foot): Errors
Tandem stance (non-dominant foot at back): Errors
And / Or
Tandem gait6,7
Time (best of 4 trials): seconds
6
Coordination examination
Upper limb coordination
Which arm was tested: Left Right
Coordination score of 1
7
Neck Examination:
Range of motion T enderness U pper and lower limb sensation & strength
Findings:
5
Scoring on the SCAT3 should not be used as a stand-alone method
to diagnose concussion, measure recovery or make decisions about
an athlete’s readiness to return to competition after concussion.
Since signs and symptoms may evolve over time, it is important to
consider repeat evaluation in the acute assessment of concussion.
260
Downloaded from bjsm.bmj.com on August 4, 2014 - Published by group.bmj.com
SCAT3 Sport Concuss ion Ass esment Tool 3 | Page 3 © 2013 Concussion in Sport Group
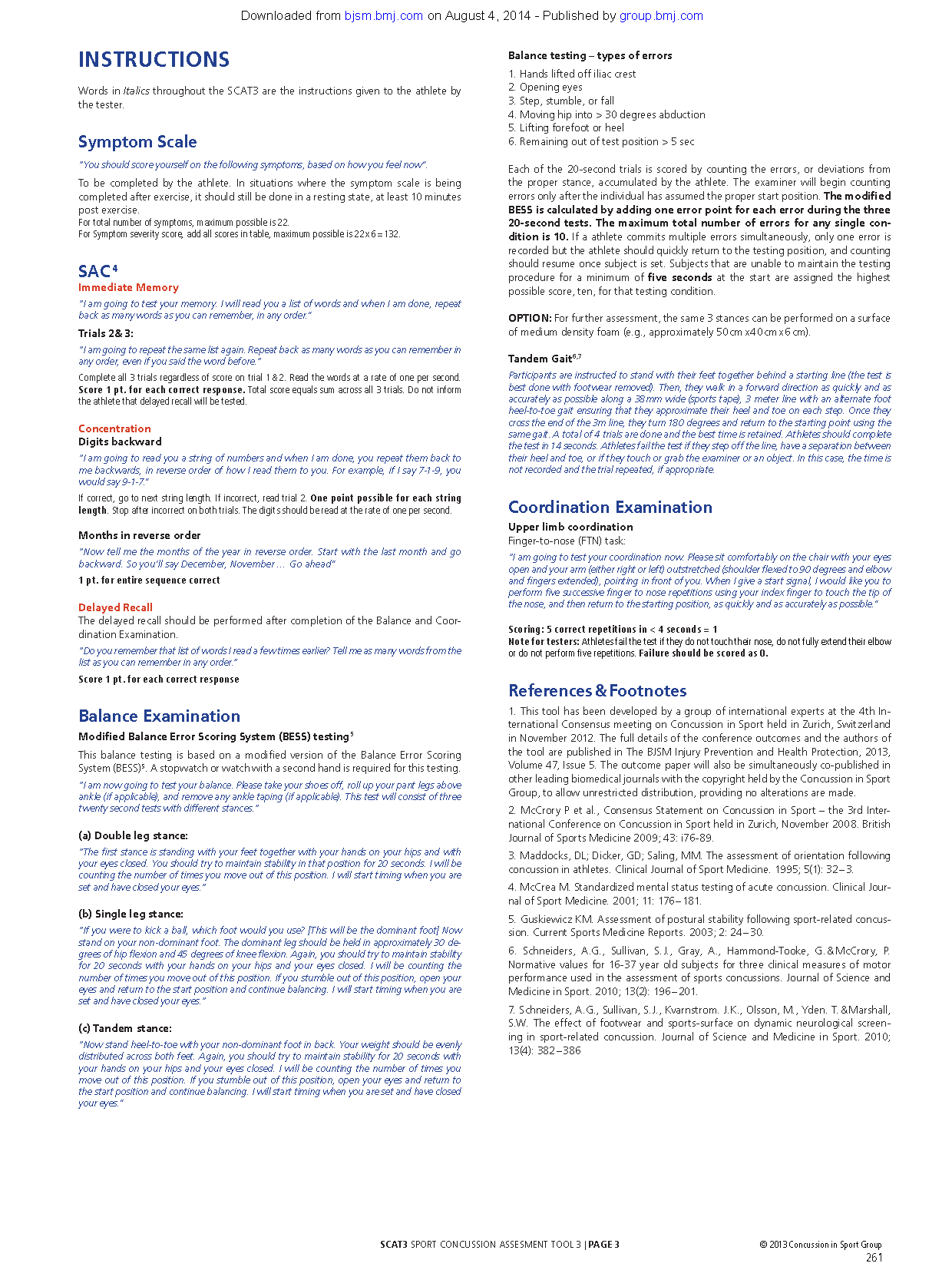
Instructions
Words in Italics throughout the SCAT3 are the instructions given to the athlete by
the tester.
Symptom Scale
“You should score yourself on the following symptoms, based on how you feel now”.
To be completed by the athlete. In situations where the symptom scale is being
completed after exercise, it should still be done in a resting state, at least 10 minutes
post exercise.
For total number of symptoms, maximum possible is 22.
For Symptom severity score, add all scores in table, maximum possible is 22 x 6 = 132.
SAC 4
Immediate Memory
“I am going to test your memory. I will read you a list of words and when I am done, repeat
back as many words as you can remember, in any order.”
Trials 2 & 3:
“I am going to repeat the same list again. Repeat back as many words as you can remember in
any order, even if you said the word before.“
Complete all 3 trials regardless of score on trial 1 & 2. Read the words at a rate of one per second.
Score 1 pt. for each correct response. Total score equals sum across all 3 trials. Do not inform
the athlete that delayed recall will be tested.
Concentration
Digits backward
“I am going to read you a string of numbers and when I am done, you repeat them back to
me backwards, in reverse order of how I read them to you. For example, if I say 7-1-9, you
would say 9-1-7.”
If correct, go to next string length. If incorrect, read trial 2. One point possible for each string
length. Stop after incorrect on both trials. The digits should be read at the rate of one per second.
Months in reverse order
“Now tell me the months of the year in reverse order. Start with the last month and go
backward. So you’ll say December, November … Go ahead”
1 pt. for entire sequence correct
Delayed Recall
The delayed recall should be performed after completion of the Balance and Coordination
Examination.
“Do you remember that list of words I read a few times earlier? Tell me as many words from the
list as you can remember in any order.“
Score 1 pt. for each correct response
Balance Examination
Modified Balance Error Scoring System (BESS) testing 5
This balance testing is based on a modified version of the Balance Error Scoring
System (BESS)5. A stopwatch or watch with a second hand is required for this testing.
“I am now going to test your balance. Please take your shoes off, roll up your pant legs above
ankle (if applicable), and remove any ankle taping (if applicable). This test will consist of three
twenty second tests with different stances.“
(a) Double leg stance:
“The first stance is standing with your feet together with your hands on your hips and with
your eyes closed. You should try to maintain stability in that position for 20 seconds. I will be
counting the number of times you move out of this position. I will start timing when you are
set and have closed your eyes.“
(b) Single leg stance:
“If you were to kick a ball, which foot would you use? [This will be the dominant foot] Now
stand on your non-dominant foot. The dominant leg should be held in approximately 30 degrees
of hip flexion and 45 degrees of knee flexion. Again, you should try to maintain stability
for 20 seconds with your hands on your hips and your eyes closed. I will be counting the
number of times you move out of this position. If you stumble out of this position, open your
eyes and return to the start position and continue balancing. I will start timing when you are
set and have closed your eyes.“
(c) Tandem stance:
“Now stand heel-to-toe with your non-dominant foot in back. Your weight should be evenly
distributed across both feet. Again, you should try to maintain stability for 20 seconds with
your hands on your hips and your eyes closed. I will be counting the number of times you
move out of this position. If you stumble out of this position, open your eyes and return to
the start position and continue balancing. I will start timing when you are set and have closed
your eyes.”
Balance testing – types of errors
1. Hands lifted off iliac crest
2. Opening eyes
3. Step, stumble, or fall
4. Moving hip into > 30 degrees abduction
5. Lifting forefoot or heel
6. Remaining out of test position > 5 sec
Each of the 20-second trials is scored by counting the errors, or deviations from
the proper stance, accumulated by the athlete. The examiner will begin counting
errors only after the individual has assumed the proper start position. The modified
BESS is calculated by adding one error point for each error during the three
20-second tests. The maximum total number of errors for any single condition
is 10. If a athlete commits multiple errors simultaneously, only one error is
recorded but the athlete should quickly return to the testing position, and counting
should resume once subject is set. Subjects that are unable to maintain the testing
procedure for a minimum of five seconds at the start are assigned the highest
possible score, ten, for that testing condition.
OPTION : For further assessment, the same 3 stances can be performed on a surface
of medium density foam (e.g., approximately 50 cm x 40 cm x 6 cm).
Tandem Gait6,7
Participants are instructed to stand with their feet together behind a starting line (the test is
best done with footwear removed). Then, they walk in a forward direction as quickly and as
accurately as possible along a 38mm wide (sports tape), 3 meter line with an alternate foot
heel-to-toe gait ensuring that they approximate their heel and toe on each step. Once they
cross the end of the 3m line, they turn 180 degrees and return to the starting point using the
same gait. A total of 4 trials are done and the best time is retained. Athletes should complete
the test in 14 seconds. Athletes fail the test if they step off the line, have a separation between
their heel and toe, or if they touch or grab the examiner or an object. In this case, the time is
not recorded and the trial repeated, if appropriate.
Coordination Examination
Upper limb coordination
Finger-to-nose (FTN) task:
“I am going to test your coordination now. Please sit comfortably on the chair with your eyes
open and your arm (either right or left) outstretched (shoulder flexed to 90 degrees and elbow
and fingers extended), pointing in front of you. When I give a start signal, I would like you to
perform five successive finger to nose repetitions using your index finger to touch the tip of
the nose, and then return to the starting position, as quickly and as accurately as possible.”
Scoring: 5 correct repetitions in < 4 seconds = 1
Note for testers: Athletes fail the test if they do not touch their nose, do not fully extend their elbow
or do not perform five repetitions. Failure should be scored as 0.
References & Footnotes
1. This tool has been developed by a group of international experts at the 4th International
Consensus meeting on Concussion in Sport held in Zurich, Switzerland
in November 2012. The full details of the conference outcomes and the authors of
the tool are published in The BJSM Injury Prevention and Health Protection, 2013,
Volume 47, Issue 5. The outcome paper will also be simultaneously co-published in
other leading biomedical journals with the copyright held by the Concussion in Sport
Group, to allow unrestricted distribution, providing no alterations are made.
2. McCrory P et al., Consensus Statement on Concussion in Sport – the 3rd International
Conference on Concussion in Sport held in Zurich, November 2008. British
Journal of Sports Medicine 2009; 43: i76-89.
3. Maddocks, DL; Dicker, GD; Saling, MM . The assessment of orientation following
concussion in athletes. Clinical Journal of Sport Medicine. 1995; 5(1): 32 – 3.
4. McCrea M. Standardized mental status testing of acute concussion. Clinical Journal
of Sport Medicine. 2001; 11: 176 – 181.
5. Guskiewicz KM. Assessment of postural stability following sport-related concussion.
Current Sports Medicine Reports. 2003; 2: 24 – 30.
6. Schneiders, A.G., Sullivan, S.J., Gray, A., Hammond-Tooke, G. & M cCrory, P.
Normative values for 16-37 year old subjects for three clinical measures of motor
performance used in the assessment of sports concussions. Journal of Science and
Medicine in Sport. 2010; 13(2): 196 – 201.
7. Schneiders, A.G., Sullivan, S.J., Kvarnstrom. J.K., Olsson, M., Yden. T. & M arshall,
S.W. The effect of footwear and sports-surface on dynamic neurological screening
in sport-related concussion. Journal of Science and Medicine in Sport. 2010;
13(4): 382 – 386
261
Downloaded from bjsm.bmj.com on August 4, 2014 - Published by group.bmj.com
SCAT3 Sport Concuss ion Ass esment Tool 3 | Page 4 © 2013 Concussion in Sport Group
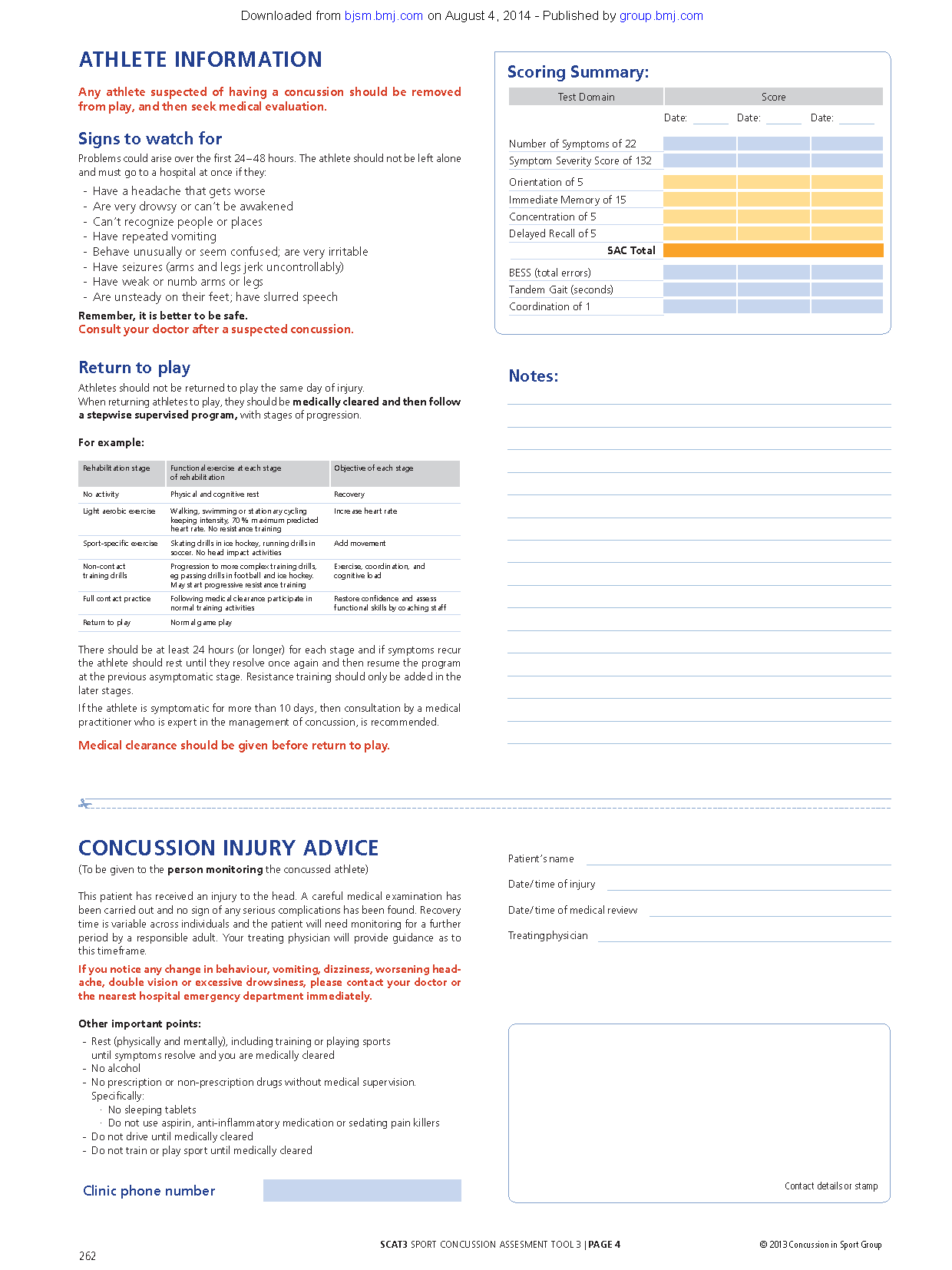
Athlete Informat ion
Any athlete suspected of having a concussion should be removed
from play, and then seek medical evaluation.
Signs to watch for
Problems could arise over the first 24 – 48 hours. The athlete should not be left alone
and must go to a hospital at once if they:
-- Have a headache that gets worse
-- Are very drowsy or can’t be awakened
-- Can’t recognize people or places
-- Have repeated vomiting
-- Behave unusually or seem confused; are very irritable
-- Have seizures (arms and legs jerk uncontrollably)
-- Have weak or numb arms or legs
-- Are unsteady on their feet; have slurred speech
Remember, it is better to be safe.
Consult your doctor after a suspected concussion.
Return to play
Athletes should not be returned to play the same day of injury.
When returning athletes to play, they should be medically cleared and then follow
a stepwise supervised program, with stages of progression.
For example:
Rehabilitation stage Functional exercise at each stage
of rehabilitation
Objective of each stage
No activity Physical and cognitive rest Recovery
Light aerobic exercise Walking, swimming or stationary cycling
keeping intensity, 70 % maximum predicted
heart rate. No resistance training
Increase heart rate
Sport-specific exercise Skating drills in ice hockey, running drills in
soccer. No head impact activities
Add movement
Non-contact
training drills
Progression to more complex training drills,
eg passing drills in football and ice hockey.
May start progressive resistance training
Exercise, coordination, and
cognitive load
Full contact practice Following medical clearance participate in
normal training activities
Restore confidence and assess
functional skills by coaching staff
Return to play Normal game play
There should be at least 24 hours (or longer) for each stage and if symptoms recur
the athlete should rest until they resolve once again and then resume the program
at the previous asymptomatic stage. Resistance training should only be added in the
later stages.
If the athlete is symptomatic for more than 10 days, then consultation by a medical
practitioner who is expert in the management of concussion, is recommended.
Medical clearance should be given before return to play.
Notes:
Concussion injury advice
(To be given to the person monitoring the concussed athlete)
This patient has received an injury to the head. A careful medical examination has
been carried out and no sign of any serious complications has been found. Recovery
time is variable across individuals and the patient will need monitoring for a further
period by a responsible adult. Your treating physician will provide guidance as to
this timeframe.
If you notice any change in behaviour, vomiting, dizziness, worsening headache,
double vision or excessive drowsiness, please contact your doctor or
the nearest hospital emergency department immediately.
Other important points:
-- Rest (physically and mentally), including training or playing sports
until symptoms resolve and you are medically cleared
-- No alcohol
-- No prescription or non-prescription drugs without medical supervision.
Specifically:
·· No sleeping tablets
·· Do not use aspirin, anti-inflammatory medication or sedating pain killers
-- Do not drive until medically cleared
-- Do not train or play sport until medically cleared
Clinic phone number
Patient’s name
Date / time of injury
Date / time of medical review
Treating physician
Contact details or stamp
Scoring Summary:
Test Domain Score
Date: Date: Date:
Number of Symptoms of 22
Symptom Severity Score of 132
Orientation of 5
Immediate Memory of 15
Concentration of 5
Delayed Recall of 5
SAC Total
BESS (total errors)
Tandem Gait (seconds)
Coordination of 1
262
Downloaded from bjsm.bmj.com on August 4, 2014 - Published by group.bmj.com
Br J Sports Med 2013 47: 259
SCAT3
http://bjsm.bmj.com/content/47/5/259.citation
Updated information and services can be found at:
These include:
References
http://bjsm.bmj.com/content/47/5/259.citation#related-urls
Article cited in:
service
Email alerting
the box at the top right corner of the online article.
Receive free email alerts when new articles cite this article. Sign up in
Collections
Topic
• Trauma CNS / PNS (113 articles)
• Trauma (738 articles)
• Injury (818 articles)
Articles on similar topics can be found in the following collections
Notes
http://group.bmj.com/group/rights-licensing/permissions
To request permissions go to:
http://journals.bmj.com/cgi/reprintform
To order reprints go to:
http://group.bmj.com/subscribe/
To subscribe to BMJ go to:
Downloaded from bjsm.bmj.com on August 4, 2014 - Published by group.bmj.com